Maintaining the dental health of patients who have been treated with full course radiotherapy of head and neck tumors is a difficult and lifelong challenge. Topical fluorides have used effectively since the 1960’s. In recent times the calcium phosphate remineralizing preparations have become available and have made a significant impact on the dental health of these patients. Patient compliance, however remains the most significant challenge in oral health maintenance in postradiation patients. This program discusses the philosophies developed at UCLA to prevent and treat postradiation disease including restorative care, endodontic therapy and postradiation extraction.
Maxillofacial Prosthetics – Maintenance, Restorative Care and Postradiation Dental Disease — Course Transcript
- 1. 6. Dental Maintenance and Restorative Care; Postradiation Dental Disease John Beumer III, DDS, MS Eric Sung, DDSDivision of Advanced Prosthodontics, Biomaterials and Hospital Dentistry and UCLA School of Dentistry All rights reserved. This program of instruction is covered by copyright ©. No part of this program of instruction may be reproduced, recorded, or transmitted, by any means, electronic, digital, photographic, mechanical, etc., or by any information storage or retrieval system, without prior permission of the authors.
- 2. Dental Maintenance Topical fluoride applications Calcium phosphate remineralizing agents Hygiene instruction Regular followup Dental prophylaxsis every four months)
- 3. Topical fluoride applicationsTopical fluorides have been used to prevent caries inpatients with radiation induced xerostomia since the1960’s (Driezen et al, 1977; Horiot et al, 1983;Jansma et al, 1989) Topical fluoride applications have been shown to prevent new caries Topical fluoride applications have been shown to arrest existing lesions
- 4. Topical Fluoride –Means of Application Mouth rinse Toothpaste Gel applied with custom carriers We recommend the use of a neutral fluoride gel applied with custom carriers and a five minute daily application.Rationale:a) Using this method, fluoride levels increase 3 fold (Bocter R, 1986)b) Better compliance
- 5. Fluoride level and biopsy depth* Fluoride (ppm) Biopsy Depth (microns) Standard Standard Visit Mean Deviation Mean Deviation Baseline 605 208 9.437 3.600 7-10 days *992 413 9.98 3.000 3 months later *1569 542 10.39 3.067 6 months later *1932 554 10.28 2.57*Boctor R, The topical use of stannous fluoride as a preventativemeasure for head and neck cancer. Master’s Thesis, 1986, UCLA**In this study a stannous fluoride gel was applied with customcarriers.
- 6. Topical Fluoride – Mechanism of Action Upon demineralization, fluoride ions in presence of calcium and phosphate ions unite to form fluorapatite (Cate, 1999) In existing carious lesions, the presence of fluoride is highly effective in accelerating remineralization Remineralization has been shown even in patients with advanced radiation caries (Driezen et al, 1977) Remineralization of subsurface lesions may be enhanced with the use of casein based phosphopeptide-amorphous calcium phosphate
- 7. Topical Fluoride – Key Facts to Remember Uptake is a surface phenomenon confined to outer 30-50 microns. Penetration is compromised by the presence of plaque. Fluoride fails to form stable compounds in the oral environment and much is lost within 24 hours. Therefore, daily applications must be employed to maintain therapeutic levels.
- 8. Topical fluoride applicationsBiggest challenge: Patient compliance. In one report only 43% of patients with radiation induced xerostomia used their fluoride daily as directed (Epstein et al, 1995) However, of the patients seen on regular followup 68% used fluoride as directed (Epstein et al, 1995)
- 9. Topical Fluoride – Key Facts to Remember Remineralized lesions with fluorapatite are more resistant than the original enamel surface Incorporation of fluoride into the apatite crystal reduces the solubility of apatite by a factor of 10 Surface layer of fluorapatite is best Until cavitation fluorapatite crystals can grow The changes in microflora persist and the risk of an aggressive caries attack remains indefinitely (Keene et al, 1981).
- 10. Topical Fluoride – Key Facts to RememberAcidulated phosphate fluorides are not recommendedfor daily applications because its low PH: Dissolves the tooth surface Daily applications will etch glazed porcelains (Copps et al, 1980) Leads to gingival and mucosal irritation in some patients affecting compliance As a result most clinicians recommend the use of neutral preparations (Vissink et al, 2003)
- 11. Calcium Phosphate Remineralizing Agents(Johansen and Sobel, 1978;Reynolds et al, 1995; Reynolds et al,2003 Papas et al, 2008; Reynolds et al, 2008; Manton et al, 2008) Amorphous calcium phosphate preparations vs Casein based calcium phosphate preparations
- 12. Calcium Phosphate Remineralizing Agents Amorphous calcium phosphate preparations** (Papas et al, 2008) Separate preparations of ammonium phosphate and calcium sulfate are deposited introrally via a dual chamber device. They dissolve in saliva and release calcium and phosphate ions In the presence of fluoride ions, amorphous calcium fluoride phosphate is precipitated This compound is very unstable and rapidly transforms into fluorhyroxyapatite**Some authors have expressed concern that since the unstabilized form ofamorphous calcium phosphate rapidly transforms into crystalline phases it mayact to promote calculus formation (Reynolds, 2008).
- 13. Calcium Phosphate Remineralizing AgentsCasein based calcium phosphate preparations The casein phosphopeptides (CPP) stabilize high concentrations of calcium and phosphate ions (ACP) and fluoride ions at the surface of the tooth by adhering to plaque and the pellicle. The calcium, phosphate and fluoride ions are stabilized by the CPP preventing the formation of calculus. However, these ions diffuse down concentration gradients into subsurface carious lesions promoting remineralization (Reynolds, 2008).
- 14. Calcium Phosphate Remineralizing AgentsCasein based calcium phosphate preparations These CPP-ACP nanocomplexes have shown to be effective when incorporated within mouth rinses, chewing gum and tooth paste (Reynolds et al, 1995; Reynolds et al, 2003) and appear to work synergistically with fluoride. Fluoride alone appears to promote remineralization of the surface whereas CCP-ACP with fluoride promotes remineralization throughout the body of the lesion.
- 15. Summary Patients should begin the use of daily topical fluoride applications immediately. This should be accompanied by the use of a remineralization paste and if available, a remineralizing chewing gum. We suggest that the daily fluoride applications be made an hour or so before bedtime. The remineralizing paste can be used at any time during the day.
- 16. Summary Fluoride tooth pastes should be employed for normal brushing. Remineralizing chewing gum should be used during daytime hours. For optimal effect the chewing gum is used four times per day and chewing sustained for 20 minutes each time (Manton et al, 2008). Patients should be followed every three months and hygiene instruction be reinforced at each followup visit. If reasonably compliant almost all patients should be able to maintain healthy dentitions.
- 17. Dietary Instructions Eliminatesucrose from the diet Reduce frequency of meals
- 18. Dietary Instructions Sucrose gel formed on tooth surfaces protects Streptococcus mutans from salivary buffering Thick gel leads to lower plague PH
- 19. Postradiation Dental Disease What are the options when a patient presents with advanced dental disease, i.e., severe periodontal disease* (deep pockets, furcation involvement), perapical pathosis or advanced caries, associated with teeth within the field? Role of postradiation extraction Role of endodontic therapy Role of restorative dentistry Periodontal therapies****Most periodontal procedures predispose the patient to great riskof perforation of the epithelial attachment and thereforeosteoradionecrosis, and are ill advised in this patient population.
- 20. Post radiation extractionsThe risk of postradiation extractions leading to ORN hasbeen a matter of debate for many years. Some authors have proposed that postradiation extractions pose little risk of precipitating an ORN (Solomon et al, 1968; Carl et al, 1973; Maxymiw et al, 1991) Others suggest that postradiation extractions create a significant risk ( Daly and Drane, 1972; Murray et al, 1980; Morrish et al, 1981; Beumer et al, 1983; Marks et al, 1985; Thorn et al, 2000)
- 21. Postradiation extraction of teeth within the radiation treatment volume – MandibleAll four of these patients presented with squamouscarcinomas of either the oral tongue or floor of the mouthand were treated with external beam photons and opposedmandibular fields. All received in excess of 6600 cGy anddeveloped ORN after postradiation extractions.All patients developed ORN before the introduction of hyperbaric oxygen andall eventually had major portions of their mandibles resected resulting indiscontinuity defects in order to control the infection.
- 22. Post radiation extractions We believe the truth lies somewhere in between these two positions. The primary risk factors are dose and the volume of tissues (gross tumor volume) exposed to the high dose levels.
- 23. Postradiation extractions* Limits of the data No prospective data Data is retrospective and mostly in the form of chart reviews Radiation doses and fields frequently not reported. As a result, clinicians responsible for determining whether postradiation extractions are appropriate must rely on clinical case series data and an in depth knowledge and understanding of the literature and the biologic effects of radiation as the best level of evidence to assist in management decisions
- 24. Postradiation extractions* Incidence of osteoradionecrosis secondary to postradiation extractions Patients Osteos Grant and Fletcher, 1966 16 7 44% Beumer et al, 1984 40 11 28% Morrish et al, 1980 18 11 61% Marx, et al, 1984 37 11 30% Totals 111 40 36%*In these clinical reports the tumor dose was in excessof 6500 cGy and the patients did not receive HBO. HBO
- 25. Post radiation extractions – Maxilla Permitted in the maxilla in most situations regardless of dose. The exception is if the sites are in the high dose range and the patient was treated with ChemoRT In these instances Hyperbaric oxygen is recommended prior to and after the extractions (per the Marx protocol, Marx et al, 1984) Consider the pentoxifylline-tocopherol protocol
- 26. Postradiation extraction – Maxilla Case studiesBoth these osteos developed following extraction of teeth afterradiation therapy. Both patients received in excess of 6600 cGyto the extraction sites. Conservative treatment was employed(local irrigation, removal of loose sequestra of bone etc.) andboth healed several months after onset. onset
- 27. Post radiation extractions – MandibleFor purposes of discussion we like to dividepostradiation extraction sites of the mandible intothree categories High dose sites – BED of 6500 cGy and above Intermediate dose sites – BED between 5500 and 6500 cGy Low dose sites – BED 5500 cGy and below
- 28. Post radiation extractions – Mandible Low dose sites Teeth can be removed with little risk of ORN However, teeth should be removed atraumatically with minimal reflection of the periosteum, from which most of the blood supply to underlying bone is derived
- 29. Postradiation extractions – Mandible High dose sites In the mandible if the dose to bone locally is above 6500 cGy consider: Hyperbaric oxygen (Marx et al, 1984). Pentoxifylline – tocopheroal protocol (Delanian et al, 2005 and Lyons and Ghazali, 2008)
- 30. Hyperbaric Oxygen Protocol (per Marx) ThirtyHBO treatments (2.4 atmospheres, 100% oxygen for 90 minutes) Following dental extractions another 10 treatments are administered.
- 31. Pentoxifylline – Tocopherol protocolPentoxifylline (400 mg bid 8 weeks prior to extractions) A vasodilator and facilitates blood flow by decreasing platelet aggregation and thrombus formation Inhibits fibrosisTocopherol (1000 IU daily beginning one week before extractions) A free radical scavenger
- 32. Post radiation extractions – Mandible Intermediate dose levels Individual patient factors are important to consider such as: Continued tobacco use Chemoradiation Clinical signs Amount of mandibular body within the gross tumor volume History of a radical neck dissectionThese factors increase the biologically equivalentdose (BED) and increase the risk of ORN
- 33. Intermediate dose sites plus individual patient factorsWe recommend considering either Hyperbaric oxygen (Marx et al, 1984). Pentoxifylline – tocopheroal protocol (Delanian et al, 2005 and Lyons and Ghazali, 2008) . . . .in association with extraction.
- 34. Rationale for Endodontic TreatmentFor mandibular teeth if the dose to bone is above5500 cGy endodontic therapy is a viablealternative to extraction (Seto et al, 1986) becauseit minimizes the risk of bone exposure The response to treatment has been favorable (healing or stabilization of the periapical pathosis). There have been no reported incidents of osteoradionecrosis resulting from endodontic procedures. The alternative to endo at doses to bone exceeding 5500 cGy (extraction plus HBO) is expensive and time consuming.
- 35. What is the role of endodontic therapy? Fortreatment of periapical disease When combined with crown amputation it also is a means of eliminating deep periodontal pockets Used when risk of ORN secondary to postradiation extraction is high (dose to bone of over 6500 cGy)
- 36. What is the role of endodontic therapy? Note that in this patient the crown has been amputated and the furcation has been exposed.
- 37. Endodontic Procedures Technical Challenges Severe trismus Narrowing of the canals Difficulty in using the rubber dam because of the extent of gingival caries File aspiration due to impaired pharyngeal reflexes
- 38. Endodontic Procedures Technical tips Short fills better than long fills Buccal access sometimes required Occlusal reduction facilitates access Floss should be tied to files to prevent aspiration Glass ionomer can be used to build up teeth to stabilize the rubber dam clamp Bend instruments at the noncutting portion of the shaft.
- 39. Role of Endodontics Patient presented with separate periodontal and periapical infections associated with the lower molar. The area had received 6800 cGy. Root canal was completed, the crown amputated and the furcation exposed.Periodontal pockets were shortened, the furcation area exposedand the infection resolved. Eventually the root fragments willexfoliate although it could take several years. Mucosal integritywas maintained.
- 40. Role of EndodonticsThis patient received 6800 cGy via opposedmandibular fields for a squamous carcinoma ofthe lateral tongue and floor of the mouth.Endodontic therapy was used to gain access to thefurcation area for oral hygiene. Eventually, the tworoots exfoliated, leaving the mucoperiosteum intact.
- 41. Treatment Options: Endodontics vs Extraction** Summary Mandibular teeth within the gross tumor volume with dose to bone above 5500 cGy. Endodontic therapy is preferred Mandibular teeth within the gross tumor volume with dose to bone below 5500 cGy Both endo and extraction are appropriate options Mandibular teeth out of the gross tumor volume Both endo and extraction are appropriate options Maxillary teeth both in and out of within the gross tumor volume Both endo and extraction are appropriate options **Extractions not accompanied by HBO.Useful guidelines only if conventional fractionation is used. Not applicable if thepatient receives adjuvant or comcomitant chemotherapy.
- 42. Postradiation Restorative Dentistry Radiation Caries The changes in microflora persist and the risk of an aggressive caries attack remains indefinitely (Keene et al, 1981). Most lesions occur in the gingival third of the teeth and in areas with extensive abrasion in which dentin is exposed such as the incisal or occlusal surfaces.
- 43. Postradiation Restorative Dentistry Radiation Caries Cervical lesions may involve the entire circumference of the teeth, eventually leading to amputation of the crown. Incisal lesions can progress rapidly and soon involve the entire crown and result in a brownish black discoloration. The histopathology of these lesions has been found to be identical to caries in nonirradiated patients (Frank et al, 1965).
- 44. Postradiation Restorative Dentistry Radiation Caries – Caries Control Remove all caries and restore the affected teeth with temporary restorations using a remineralizing restorative material (IRM-Dentsply-Caulk) Reinstitute the use of topical fluoride in combination with remineralizing pastes and chewing gum. If the lesion is limited, it may not require placement of a temporary restoration. Once caries has been controlled, the temporary restorative material is replaced with amalgam, composite or glass ionomer.
- 45. Postradiation Operative Dentistry Restorative materials – Posterior Restorations Amalgam is preferred since these restorations can be extended if recurrent decay develops. Also, amalgam restorations are less sensitive to moisture contamination and polished amalgams promote better tissue responses.
- 46. Post-radiation dental treatmentWhen preparing the teeth to receive amalgam restorations Avoid trauma from rubber dam clamps Pulp capping NOT recommended if teeth received radiation doses in excess of 5500 cGy Extensive caries: Don’t remove unsupported enamel
- 47. Postradiation Operative DentistryRestorative Materials – Anterior Restorations Composite restorations – Limitations During cavity preparation margins frequently terminate in dentin or cementum and, as a result, the risk of subsequent microleakage and recurrent decay is high. Moisture control is frequently less than optimal due to difficulty in controlling gingival hemorrhage.
- 48. Postradiation Operative DentistryRestorative Materials – Anterior Restorations Composite restorations – Limitations In small lesions glass ionomer cements (GIC’s) may be preferred. Although microleakage is a significant problem with this material, GIC’s are ion releasing and when fluoride is incorporated within the material, it is slowly released resulting is an anticaries effect. Recently, casein phosphopeptide-amorphous calcium phosphate nanocomplexes have been incorporated within GIC’s (Mazzaoui et al, 2003). The effectiveness of ion release in these patients is unknown
- 49. Post-radiation dental treatment Full coverage restorations: Good oral hygiene Abutment teeth for RPD’s Esthetic concerns Adequate hygiene access Sub-gingival margins
- 50. Postradiation Fixed Prosthodontics Risks and PrecautionsRecurrent caries at the marginsIatrogenic trauma may cause an osteoradionecrosisAvoid acidulated fluoride solutions since they will etch glazed porcelain.Subgingival margins when possibleAvoid perforating the epithelial attachment of teeth within the radiation field when packing gingival retraction cord
- 51. Postradiation Fixed ProsthodonticsCast restorations should be used onlywhen the following conditions are met: Excellent oral hygiene is exhibited There is inadequate tooth structure for intracoronal restorations Itis necessary as an abutment for fixed or removable partial dentures Adequate working space is available
- 52. Postradiation Operative Dentistry Technical aspects: Dueto extensiveness of caries it is not always appropriate to remove unsupported enamel. Pulp capping is not recommended due to the poor reparative potential of the irradiated dental pulp. Inlarge cervical caries, preparations and restorations can be done incrementally to ease difficulty in placing restorative material in unsupported cavity preparations. Avoid trauma with the rubber dam clamp.
- 53. Postradiation Operative Dentistry Technical aspects: If caries extends interproximally as well as buccally and lingually in posterior teeth, a conventional MOD restoration is placed initially taking care to extend the restoration subgingivally. At a subsequent appointment the buccal and/or lingual amalgam restorations are placed. Sequential restoration of circumferential lesions is advisable in anterior teeth. With large Class V restorations, restore approximately one half of the gingival area at the first appointment and restore the remaining gingival portion subsequently. If the caries extends into interproximal areas, placing of a small section of matrix band with a suitable interproximal wedge will simplify and improve the condensation of the amalgam.
- 54. Visit ffofr.org for hundreds of additional lectures on Complete Dentures, Implant Dentistry, Removable Partial Dentures, Esthetic Dentistry and Maxillofacial Prosthetics. The lectures are free. Our objective is to create the best and most comprehensive online programs of instruction in Prosthodontics
- 55. References Johansen E, Sobel S. (1978) Dental management of patients with head and neck cancer. Presented at the annual meeting of the American Radium Society, New Orleans. Reynolds E, Cain C, Webber F, et al. (1995) Anticariogenicity of calcium phosphate complexes of tryptic casein phosphopeptide-amorphous calcium phosphate nanocomplexes in the rat. J Dent Res 74:1272-79. Papas A, Russel D, Singh M, et al. (2008) Caries clinical trial of a remineralizing toothpaste in radiation patients. Gerondontology 25:76-88. Reynolds E, Cai F, Shen P, et al. (2003) Retention in plague and remineralization of enamel lesions by various forms of calcium in a mouthrinse or sugar-free chewing gum J Dent Res 82:206-11. Frank R, Herdly J, Philippe E. (1965) Acquired dental defects and salivary gland lesions after irradiation for carcinoma. J Amer Dent Assoc 70:868-83. Mazzaoui S, Burrow M, Tyas M, et al. (2003) Incorporation of casein phosphopeptide-amorphous calcium phosphate into glass ionomer cement. J Dent Res 82:914-18. Seto B, Beumer J, Kagawa T, et al. (1986) Analysis of endodontic therapy in patients irradiated for head and neck cancer. Oral Surg Oral Med Oral Path 60:540-5.
- 56. References Solomon H, Marchetta F, William R, Miller R, et al. (1968) Extraction of teeth after cancercidal doses of radiation therapy to the head and neck. Am J Surg 115:349-51. Carl W, Schaaf N, Sako K. (1973) Oral surgery and the patient who has had radiation therapy for head and neck cancer. Oral Surg 36:651-9. Maxymiw W, Wood R, Liu F. (1991) Post-radiation dental extractions without hyperbaric oxygen. Oral Surg Oral Med Oral Path 72:270-4. Marx R, Johnson R, Kline S. (1985) Prevention of osteoradionecrosis: A randomized prospective clinical trial of hyperbaric oxygen versus penicillin. J Amer Dent Assoc 111:49-54. Delanian S, Porcher R, Balla-Mekias S, et al. (2003) Randomized placebo controlled trial of combined pentoxifylline and tocopherol for regression of superficial radiation induced fibrosis. J Clin Oncol 21:2545-50. Delanian S, Lefaix J. (2004) The radiation-induced fibroatrophic process: Therapeutic perspective via the antioxidant pathway. Radiother Oncol 73:119. Hoffmeister S, Macomber W, Wong M. (1969) Radiation in dentistry – surgical comments. J Am Dent Assoc 78:511-16. Manton D, Walker G, Cai F, et al. (2008) Remineralization of enamel subsurface lesions in situ by the use of three commercially available sugar free gums. Int J Paediatr Dent 18:284-90.
- 57. References Horiot J, Schraub S, Bone M, et al. (1983) Dental preservation in patients irradiated for head and neck tumors: A ten year experience with topical fluoride and a randomized clinical trial between two fluoridation methods. Radiother Oncol 1:77-82. Jansma J, Vissink A, s-Gravenmade E, et al. (1989) In vivo study on the prevention of radiation caries. Caries Res 23:172-8. ten Cate J. (1999) Current concepts on the theories of the mechanism of action of fluoride. Acta Odontol Scand 57:325-9. Reynolds E, Cai F, Cochrane N et al. (2008) Fluoride and cassein phosphopeptide-amorphous calcium phosphate. J Dent Res 87:344-8. Copps D, Lacy A, Carman J., et al. (1984) Effects of topical fluoride on six low fusing porcelains. J Prosthet Dent 52:340-3. Gron P. (1977) Chemistry of topical fluorides. Caries Res 11:172-204. Meyerowitz C, Featherstone J, Billings R et al. (1991) Use of intraoral model to evaluate 0.05% sodium fluoride mouthrinse in radiation-induced hyposalivation. J Dent Res 70:894-98. Epstein J, van der Meji E, Emerton S, et al. (1995) Compliance with fluoride gel use in irradiated patients. Spec Care Dent 15:218-22.
- 58. References Beumer J, Harrison R, Sanders B, et al. Postradiation dental extractions: a review of the literature and a report of 72 episodes. Head Neck Surg 6:581-6, 1983 Driezen S, Brown L, Daly T, et al. Prevention of xerostomia-related dental caries in irradiated cancer patients. J Dent Res 56:99-104, 1977 Montgomery, S. (1977) Endodontic complications in an irradiated patient. J Endod 3:277. Keene H, Daly T, Brown L, et al. (1981) Dental caries and streptococcus mutans prevalence in cancer patients with irradiation-induced xerostomia 1-13 years after radiotherapy. Caries Res 15:416. Keene H and Flemming T. (1987) Prevalence of caries associated microflora after radiotherapy in patients with cancer of the head and neck. Oral Surg Oral Med Oral Path 64:421.
- 59. References Epstein J, Chin E, Jacobson J, et al. The relationships among fluoride, cariogenic oral flora, and salivary flow rate during radiation therapy. Oral Surg Oral Med Oral Path Oral Radiol Endod 86:286-92, 1998 Seto B, Beumer J, Kagawa T, et al. Analysis of endodontic therapy in patients irradiated for head and neck cancer. Oral Surg Oral Med Oral Path 60:540-5, 1985 Toljanic J, Siddiqui A, Patterson G, Irwin M. An evaluation of a dentifrice containing salivary peroxidase elements for the control of gingival disease in patients irradiated for head and neck cancer. J Prosthet Dent 76:292-6, 1996
- 60. The End


 Cement Retention vs Screw Retention
Cement Retention vs Screw Retention
 Prosthodontic Procedures and Complications
Prosthodontic Procedures and Complications
 Angled Implants
Angled Implants
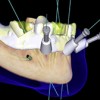 Computer Guided Treatment Planning and Surgery
Computer Guided Treatment Planning and Surgery
