Transcript of “Angled implants”
1. Dental Implants Angled (tilted) implants John Beumer III DDS, MS Allesandro Pozzi DDS Division of Advanced Prosthodontics, UCLA This program of instruc1on is protected by copyright ©. No por1on of this program of instruc1on may be reproduced, recorded or transferred by any means electronic, digital, photographic, mechanical etc., or by any informa1on storage or retrieval system, without prior permission.
2. Tilted implants ª Four implants ª Six implants ª Pterygoid implants ª Zygoma1c implants
3. Tilted Implants – Edentulous Maxilla When restoring the edentulous maxilla what does this term indicate? ª Posterior implants are 1lted distally at about a 30 degree angle and placed parallel to the anterior wall of the maxillary sinus
4. Tilted Implants – Edentulous Maxilla Why are they advantageous in the edentulous maxilla? v Longer implants in the distal posi1ons v Improved primary stability v Distal implants exit more posteriorly reducing the length of the can1lever
5. ª Eliminates the need for sinus augmenta1on ª Eliminates the need for zygoma1c implants ª Enables fabrica1on of an implant-‐supported restora1on in many pa1ents ª Enables immediate loading in selected pa1ents Tilted Implants – Edentulous Maxilla
6. Biomechanics are favorable ª More anterior – posterior (A-‐ P) spread ª Longer implants in the distal posi1ons than if placed axially ª Shorter can1levers required to restore the posterior occlusion A-‐P Spread Tilted Implants – Edentulous Maxilla Why do they work? ª Note the difference between the pa1ent’s right where implants are angled, and the leV where implants are placed axially Courtesy Dr. O. Jensen
7. Biomechanics are favorable ª Finite element analysis has shown that the use of 1lted implants is much more favorable biomechanically than using shorter implants with axial inclina1ons (Bevilacqua et al, 2010). Courtesy Dr. P. Pera Tilted Implants – Edentulous Maxilla Why do they work?
8. Success rates are above 90% (Ma^sson et al, 1999; Krekmanov et al, 2000; Malo et al, 2011; Tealdo et al, 2014). Tealdo et al (2014) has the most long term follow-‐up data. Tilted Implants – Edentulous Maxilla
9. Three approaches ª All on four (Nobel) ª Only four implants are placed ª Angled abutments used to offset the angles of the implants ª Prosthesis is placed immediately ª Columbus bridge protocol ª Four to six implants are placed ª Angled abutments used to offset the angles of the implants ª Prosthesis is placed within 24 hours ª Co-‐axis implants ª Four more implants are placed ª Co-‐axis implants are used. Angula1on correc1on is subgingival and effected by the angula1on of the implant plaborm
10. All on four – Maxilla (per Nobel) Very specific defini1on: Use of 4 implants to support an immediately loaded fixed prosthesis used to restore either the edentulous maxilla and mandible
11. All on four (per Nobel) ª Computer guided treatment planning and and fully guided implant placement is preferred What is computer guided treatment planning and surgical placement?
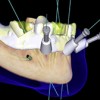
12. ª Fully guided surgery implies that the surgical templates with their drill sleeves (bushings) control the posi1on, angula1on, diameter as well as the depth of the implant osteotomy sites* ª The surgical template is secured with bone screws or anchor pins All on four (per Nobel) * See lecture en1tled computer guided treatment planning and implant surgery for details. Drill Sleeves (Bushings)
13. All on four (per Nobel) ª The prosthesis is prepared prior to implant surgery and delivered immediately aVer implant placement ª For immediate loading the implants must be anchored with sufficient primary stability to withstand occlusal func1on ª This may require that the apical por1on of the posterior implants engage the cor1cal layers of bone associated with the paranasal sinus walls.
14. All on Four – Maxilla (per Nobel) Posi1on and angula1on Conven1onal ª Anterior implants placed in the lateral-‐central interproximal regions and are parallel to one another ª Posterior implant aligned parallel to the anterior wall of the maxillary sinus ª Angled abutments are only necessary for the posterior implants
15. In efforts to improve primary implant anchorage two other implant configura1ons have been proposed (Jensen et al, 2015) M-‐4 Configura1on V-‐4 Configura1on All on Four – Maxilla (per Nobel) Posi1on and angula1on Courtesy Dr. O. Jensen
16. M-‐4 ª Four implants placed at 30 degree angles to miss nasal and sinus pneuma1zed cavi1es in an M-‐shaped configura1on when viewed on panoramic radiography (Jensen et al, 2015). All on Four – Maxilla (per Nobel) Posi1on and angula1on Courtesy Dr. O. Jensen
17. ª When abundant bone is present M-‐4 implant configura1ons in pa1ents provides excellent support of the prosthesis with 20 mm between implants. This arrangement requires li^le if any distal can1lever. ª Angled abutments are used on all four implants All on Four – Maxilla (per Nobel) Posi1on and angula1on Courtesy Dr. O. Jensen
18. ª Pa1ent with moderate resorp1on and the recommended implant posi1oning with the aim of maximizing A-‐P spread ª Angled abutments are used on all four implants ª A-‐P spread may by subop1mal in these pa1ents and unless primary implant anchorage is op1mal, loading should be delayed All on Four – Maxilla (per Nobel) Posi1on and angula1on Courtesy Dr. O. Jensen
19. V-‐4 ª The V-‐4 designa1on denotes four implants placed at 30 degree angles to miss the sinus and nasal cavi1es all converging toward the midline in a V-‐forma1on (Jensen et al, 2015). ª Angled abutments are used on all four implants All on Four – Maxilla (per Nobel) Posi1on and angula1on
20. (V-‐4 implant configura1on with trans-‐sinus implants) ª Pa1ents with advanced resorp1on. There is commonly a deficiency of bone mass such that posterior implants gain limited fixa1on in a thin lateral nasal wall. Anterior “vomer” implants are usually well fixed in the nasal crest. ª A palatal view demonstra1ng implant anchorage points. The posterior implants are directed toward maximal bone mass at the lateral pyriform, while the anterior implants are aimed toward the maximum available midline bone mass which usually extends superiorly into the nasal crest (V point). All on Four – Maxilla (per Nobel) Posi1on and angula1on Courtesy Dr. O. Jensen
21. All on four – Maxilla (per Nobel) (V-‐4 implant configura1on with trans-‐sinus implants) • Under these circumstances delayed loading is recommended Courtesy Dr. O. Jensen
22. Defini1ve prostheses All on four (per Nobel) Courtesy Dr. M. Adams Consists of a fixed hybrid prosthesis ª Resin denture teeth ª Acrylic resin ª Metal substructure imbedded within the acrylic resin
23. All on four (per Nobel) Defini1ve prostheses Consists of a fixed hybrid prosthesis ª Resin denture teeth ª Acrylic resin ª Metal substructure imbedded within the acrylic resin Courtesy Dr. M. Adams
24. All on Four (per Nobel) Defini1on: Use of 4 implants to support an immediately loaded fixed prosthesis used to restore either the edentulous maxilla and mandible Exclusionary criteria (Maxilla) ª Pa1ents with significant parafunc1onal ac1vity ª Pa1ents with severe Class II or Class III jaw rela1ons ª Anchoring the surgical drill guide is difficult ª Unfavorable biomechanics ª Pa1ents with opposing arch composed primarily of natural den11on ª It is difficult to properly control the occlusion in such pa1ents
25. As men1oned earlier the defini1on the “All on four” approach is uses 4 implants to support an immediately loaded fixed prosthesis used to restore either the edentulous maxilla and mandible What are the prerequisites for immediate loading?* All on Four (per Nobel)
26. Immediate Loading v For the implants to become osseointegrated they must remain immobilized during the healing period. v Therefore one of the keys to successful immediate loading con1nues to be the effec1veness of primary implant stability
27. Ini1al Primary Stability (First day) Func1on of: v Local bone quan1ty and quality v Implant geometry Tapered be^er than cylindrical because you have a be^er chance of maximizing bone contact with the internal and external diameters of the implant v Surgical procedure (skill) Inser1on torque – in excess of 45 N/cm ISQ’s – 70 and above Two main factors: 1. Amount of ini1al bone contact 2. Lateral compression of the osteotomy site crea1ng local compression stresses Courtesy Dr. C. Stanford
28. Immediate Loading – When Is it Feasible? The degree of ini1al bone anchorage v Skill of the surgeon. Immediate loading is not for beginners Consider bicor1cal stabiliza1on when possible You must a^empt to engage the inner and outer diameter of the implant with bone when appropriate Inser1on torque – in excess of 45 N/cm ISQ’s – 70 and above v Volume and density of the bone associated with implant site Sites with dense trabecular bone are preferred Longer implants are generally preferred Bicor1cal anchorage may be necessary Clinical issues to be considered:
29. Implant selec1on ª Tapered, self tapping with sharply pitched threads Implant placement procedure ª Semi-‐guided or fully guided is preferred over free hand prepara1on of the osteotomy site and inser1on of the implants Immediate loading All on 4 per Nobel Requirements for successful outcomes
30. Immediate loading All on 4 per Nobel Requirements for successful outcomes Assessment of implant anchorage ª Torque values -‐ 45 N/cm or more ª RFA values (resonance frequency analysis) – 70 and above ª Don’t over torque for this may impair the balance of the biologic processes associated with osseointegra1on (O’Sullivan et al, 2000; Bashutski et al 2009; Cha et al, 2015) ª Excessive levels of torque increases the zone of dead and dying osteocytes leading to increased resorp1on and a disrup1on of the balance of remodeling and repair mechanisms
31. Characteris1cs of the immediate load prosthesis* ª Rigidity and cross arch stabiliza1on ª Passive fit ª Minimize the can1lever and bending moments ª Occlusion ª Clinical remounts ª Balanced ar1cula1on * A successful outcome requires that the implants remain immobile (less than 100 microns of movement) (Maniatopoulos et al, 1986; Szmuckler-‐Moncler, 2000) during the healing phase. Immediate loading Requirements for successful outcomes
32. Compliant pa1ent ª Manipulate oral hygiene aids ª Follow postopera1ve instruc1ons. They include: ª Liquid diet for the first 3 weeks ª Frequent oral rinses with warm salt water rinses beginning 24 hours aVer surgery. ª Twice per day oral rinses with chlorhexidine beginning 4 day aVer delivery and con1nuing for 10 days. ª Mechanical soV diet for another 3 weeks. ª Avoid clenching and bruxing Immediate loading Requirements for successful outcomes
33. All on four – Maxilla (per Nobel) Why? ª The surgery is technique sensi1ve ª Requires bicor1cal stabiliza1on in many pa1ents ª Old technology and materials ª It’s a fixed prosthesis ª Poor lip and facial support ª Speech and hygiene access are oVen incompa1ble ª Requires a great deal of interocclusal space ª Esthe1cs ª Cost ª Two prostheses ª Angled abutments are expensive ª Beware of “one size fit all” approach At UCLA we believe few pa1ents are well served with this approach Courtesy Dr. M. Adams
34. All on four -‐ Maxilla Issues of concern The surgery is technique sensi1ve ª Bicor1cal stabiliza1on of implants is oVen required ª Trans sinus implants oVen required to achieve the desired amount of A-‐P spread ª High level of surgical skill required ª If you loose just one implant you loose the prostheses Courtesy Dr. O. Jensen
35. All on four – Maxilla (per Nobel) Issues of concern ª Defini1ve prosthesis (Fixed hybrid prosthesis) uses old technology and materials ª Denture teeth subject to wear and fracture ª Acrylic resin subject to wear and oral contamina1on Courtesy Dr. M. Adams
36. Issues of concern ª Defini1ve prosthesis (Fixed hybrid prosthesis) uses old technology and materials ª Denture teeth subject to wear and fracture ª Acrylic resin subject to wear and oral contamina1on All on four – Maxilla (per Nobel) Courtesy Dr. K. Lyons
37. All on four – Maxilla (per Nobel) Issues of concern ª Defini1ve prosthesis (Fixed hybrid prosthesis) uses old technology and materials ª Denture teeth subject to wear and fracture ª Acrylic resin subject to wear and oral contamina1on
38. All on four – Maxilla (per Nobel) Issues of concern ª It’s a fixed prosthesis ª Poor lip and facial support ª Speech and hygiene access are oVen incompa1ble ª Requires a great deal of interocclusal space ª If insufficient the prosthesis may not be able to withstand the rigors of func1on ª Esthe1cs – The prosthesis junc1on is designed to be superior to the smile line
39. All on four – Maxilla (per Nobel) Issues of concern -‐ Maxilla ª Esthe1cs and lack of lip support ª Pa^ern of resorp1on following loss of teeth leads to a pseudo class III jaw rela1on ª It is not possible to properly support the lip of most such pa1ents ª A denture flange is needed
40. All on four – Maxilla (per Nobel) Issues of concern ª Hygiene access and speech ar1cula1on ª When you provide hygiene access, speech ar1cula1on is compromised. ª When you close the spaces used for hygiene access to permit proper speech ar1cula1on, hygiene is compromised. Courtesy Dr. M. Adams
41. All on four – Maxilla (per Nobel) Issues of concern ª Hygiene access and speech ar1cula1on ª When you close the spaces used for hygiene access to permit proper speech ar1cula1on, hygiene is compromised. ª Note the plaque that has accumulated on the 1ssue side of this “All on Four” prosthesis Courtesy Dr. M. Adams
42. As a result many prosthodon1sts prefer the use of either implant supported or implant assisted overdentures. Advantages: ª Be^er hygiene access ª Be^er lip support ª Be^er esthe1cs ª Less costly for the pa1ent What are the alterna1ves?
43. Alterna1ve treatment Overdenture Implant assisted design ª Combined implant and soV 1ssue support ª Resilient a^achments posteriorly
44. Alterna1ve Treatment Overdenture Implant supported design ª Support derived from implants ª Milled bar with a^achments
45. All on four – Maxilla (per Nobel) Addi1onal issues of concern ª Interocclusal space ª 15-‐17mm ª Smile line ª Many clinicians using the “All on four” approach advise placing the junc1on between the prosthesis and the mucosa above the lip line during a high smile ª This may require removal of excessive amounts of bone Courtesy Dr. S. Lewis Courtesy Dr. P. Pera
46. All on four – Maxilla (per Nobel) Addi1onal issues of concern ª Interocclusal space ª 15-‐17mm ª Smile line ª Because of the design of the prosthesis, addi1onal reduc1on of bone is required if the smile line is high. One mm of addi1onal bone reduc1on necessary for every mm the smile line is above the CEJ Courtesy Dr. S. Lewis Courtesy Dr. P. Pera
47. All on four – Maxilla (per Nobel) Addi1onal issues of concern ª Interocclusal space ª 15-‐17mm ª Smile line ª We feel that there are other alterna1ves which be^er serve the pa1ent (i.e. the Columbus bridge protocol and delayed loading using metal-‐ceramic or a monolithic zirconia prosthesis) Courtesy Dr. S. Lewis Courtesy Dr. P. Pera
48. Addi1onal issues of concern ª Interocclusal space ª Fracture of the prosthesis may occuer when there is insufficient interocclusal space to fabricate a prosthesis of sufficient bulk to withstand occlusal func1on. All on four – Maxilla (per Nobel)
49. All on 4 concept – Edentulous Maxilla Overdentures may be preferred Advantages ª Implant supported ª Be^er esthe1cs ª Lip support provided by a denture flange ª Be^er speech ar1cula1on ª Be^er hygiene access
50. What about the use of 1lted implants in the edentulous mandible? May be necessary when an appropriate anterior – posterior (A-‐P) spread cannot be obtained using axial inclina1ons.
51. What is the minimal A-‐P spread necessary to fabricate a fixed prosthesis for the edentulous mandible? ª Length of implants ª Minimum length -‐ 7 mm ª Number of implants ª Minimum number -‐ 4 ª A-‐P Spread ª Minimum amount – 1 cm (A-‐P spread) (A-‐P spread)
52. Anterior – Posterior Spread and the length of the can1lever extension A-‐P Spread (1 cm or more) ª Can1lever length should not exceed 2 1mes the A-‐P spread or a maximum of 20 mm. ª When A-‐P spread is less than 1 cm it may not be possible to restore the posterior den11on because of limits of the can1lever Can9lever Length What is the minimal A-‐P spread in combina1on with the length of the can1lever, necessary to fabricate a fixed prosthesis for the edentulous mandible?
53. Anterior – Posterior Spread A-P Spread (1 cm or more) Cantilever length should not exceed 2 times the A-P spread. CantileverLength What is the minimal A-‐P spread in combina1on with the length of the can1lever, necessary to fabricate a fixed prosthesis for the edentulous mandible?
54. Consequences of insufficient A-‐P spread and excessive can1lever length Result ª Mechanical failures ª Implant overload In this pa1ent the result was recurrent fractures of the prosthesis retaining screws (arrows).
55. Insufficient A-‐P spread combined with excessive can1lever length (34 mm on the leV side and 26 mm on the right side) Result: ª Mechanical failure -‐ Implant fracture ª Implant overload and loss of bone anchoring the implant In this pa1ent a combina1on of excessive can1lever length and insufficient A-‐P spread lead to implant overload and a resorp1ve remodeling response of the adjacent bone and implant fracture. Consequences of insufficient A-‐P spread and excessive can1lever length
56. Implant Overload and Bone Resorp1on Mechanisms of Implant Failure v Excessive occlusal loads v Resul1ng microdamage (fractures, cracks, and delamina1ons [arrows]) v Resorp1on remodeling response of bone is provoked v Increased porosity of bone in the interface zone secondary to remodeling v Vicious cycle of con1nued loading, more micro-‐damage, more porosity un1l failure (Howshaw et al, 1995; Brunski et al, 2000; Myata et al, 2002; Myamoto et al, 2008; Nagasawa et al, 2013 )
57. Biomechanics and A-‐P spread – Case report ª Six implants have have been placed, A-‐P spread is only about 5 mm. The can1lever extension must be limited to 10 mm and this is insufficient to restore the posterior den11on with a fixed prosthesis. ª What would have a be^er op1on for this pa1ent?
58. Biomechanics and A-‐P spread – Case report Either ª Tilted implants with four implants and a fixed prosthesis ª Placement of two implants and an overdenture
59. Tilted implants – Mandible Pa1ent selec1on ª Pa1ents with square arch forms ª Pa1ents demonstra1ng an anterior loop of the mental nerve ª This technique will improve implant distribu1on pa^ern (increase the A-‐P spread) for more favorable biomechanics
60. Tilted implants – Mandible Uses and advantages ª Square arch forms ª Avoid the anterior loop of the inferior alveolar nerve ª Shortens the can1lever ª Minimizes the risk of biologic and mechanical failures
61. ª Anterior implants should be placed in the lateral incisor posi1ons ª Note the posi1on of these anterior implants Tilted implants – Mandible Posi1oning of implants Courtesy Dr. N. Barakat
62. In pa1ents with a Cawood Class V or VI mandible there is li^le addi1onal benefit from 1pping the posterior implants Treatment of the rely Resorbed Mandible ferior rows) e of the Under these circumstances it is best to place two implants and make an overdenture Tilted implants – Mandible
63. Exclusionary criteria ª Cawood Class V or VI mandible ª Tipping the posterior implant posterior is only valuable when there is at least 3-‐4 mm of bone over the nerve Tilted implants – Mandible Courtesy Dr. O. Jensen
64. ª Computer guided treatment planning and implant placement preferred ª The prosthesis may be delivered immediately if op1mal anchorage is achieved Tilted implants – Mandible
65. The Columbus Bridge Use of angled implants to restore the edentulous maxilla ª Only select group of pa1ent qualify ª Pa1ents with favorable jaw rela1ons and bone contours are preferred. Those with pseudo class III jaw rela1ons are not considered good candidates ª Prosthe1c volume and smile line is carefully evaluated ª 4-‐6 implants are placed ª Pterygoid implants used when necessary
66. The Columbus Bridge Use of angled implants to restore the edentulous maxilla Surgical protocol ª Tapered, self taping implants with external hex used ª Anterior implants placed in tooth posi1ons ª Implants of at least 13 mm in length are desired ª Implants placed with free hand drilling with the aid of a surgical template ª Implant inser1on torque should exceed 40 N/cm ª Angled, conical abutments are used in the posterior posi1ons ª No bone regenera1ve techniques used Courtesy Dr. P. Pera
67. The Columbus Bridge Use of angled implants to restore the edentulous maxilla ª Impressions made immediately following implant placement ª Metal framework waxed and cast based on a diagnos1c wax-‐up/ trial denture set up ª It must be sufficiently rigid to resist bending ª Rigid gold or palladium alloys are used ª The prosthesis is designed without can1levers ª The func1onal and esthe1c surfaces of the provisional are restored with denture teeth and acrylic resin ª Prosthesis is screw retained ª Prosthesis delivered within 24 hours of implant placement ª Defini1ve prosthesis fabricated 4 months following implant surgery Prosthodon1c protocol
68. The Columbus Bridge (A variant of the all on four concept) Provisional is delivered within 24 hours and is resin with a metal substructure Courtesy Dr. P. Pera
69. Finished prosthesis. Usually the provisional is replaced during the first year. The Columbus Bridge (A variant of the all on four concept) Delivery One year later Courtesy Dr. P. Pera
70. Courtesy Dr. D. Howes Subcrestal vs supracrestal angula1on correc1on However, surgical placement is more demanding Co-‐axis implants ª Co-‐axis implants are used ª Two prostheses $825 / angled abutment Subcrestal is preferred
71. Advantages of Coaxis implant ª Less cost ª Screw retained ª Prosthodon1c and technical simplicity ª Standard prosthe1c componentry Courtesy Dr. D. Howes Subcrestal vs supracrestal angula1on correc1on Angled abutments vs Coaxis implants However, surgical placement is more demanding Co-‐axis implants
72. Data – Tilted implants and immediate loading Courtesy Dr. P. Pera) Retrospec1ve studies published during the last several years and recent literature reviews (Papaspyridakos et al, 2014, Gallucci et al, 2014) appear to indicate that immediate load prostheses can be employed with success in the edentulous maxilla. However the report of Tealdo and colleagues (2014) is perhaps the most revealing.
73. ª The pa1ents were divided into two groups – an immediate load group (34 pa1ents)(prosthesis delivered within 24 hours) and a delayed loading group (15 pa1ents) (prosthesis delivered an average of 8.75 months aVer implant placement). The groups were unmatched. ª All implants used in the study had acid etched surfaces, were 4 mm in diameter and at least 10 mm in length. Straight walled implants were placed into healed edentulous sites and tapered implants placed into extrac1on sites. ª Four to six implants were placed in the immediate load group, the distal implants were 1lted distally and all implants achieved inser1on torques of at least 40 Ncm. Data – Tilted implants and immediate loading Courtesy Dr. P. Pera)
74. ª The prostheses for the immediate load pa1ents were designed without distal can1levers, customized metal frameworks were fabricated of palladium alloy, occlusal surfaces were restored with resin, and the occlusal scheme used was group func1on. ª Reproducible periapical radiographs using customized film holders were obtained at delivery and at subsequent 12 month intervals in order to assess bone levels around the implants. ª The cumula1ve implant survival rate was 93.9% for the immediate load group and 95.9% for the delayed load group. No pa1ent lost more than one implant. In both groups, almost all of the implant losses were within 12 months of implant placement. Data – Tilted implants and immediate loading Courtesy Dr. P. Pera)
75. ª All original fixed prostheses remained in func1on but several required altera1ons or repairs, most secondary to fractures associated with the resin veneers. However there were no fractures associated with the metal frameworks. ª Mean bone loss around implants was greater for the delayed group than for the immediate load group. Data – Tilted implants and immediate loading Courtesy Dr. P. Pera)
76. All on 6 with Pterygoid Implants Preferred when opposing mandible is dentate
77. With guided workup and surgical procedures the prosthesis can be designed and fabricated prior to implant placement All on 6 with Pterygoid Implants
78. ª Avoids sinus augmenta1on ª Improves implant distribu1on pa^erns, A-‐P spread and biomechanics ª Preferred if immediate loading is considered ª Success rates of pterygoid implants close to 90% (Candel et al, 2012) All on 6 with Pterygoid Implants
79. ª Used to provide posterior support in full arch and posterior quadrant prostheses ª Success rates close to 90% (Candel et al, 2012) All on 6 with Pterygoid Implants
80. All on 6 with Pterygoid Implants
81. All on 6 with Pterygoid Implants ª Framework is made of monolithic zirconia ª Crowns are made of lithium disilicate and cemented to the framework
82. Tilted implants -‐ Posterior quadrants ª An alterna1ve to sinus augmenta1on ª Computer guided treatment planning and implant placement is preferred
83. Tilted implants -‐ Posterior quadrants • Anterior guidance provided by natural den11on
84. Pterygoid implants ª Combina1on of 1lted and pterygoid implant ª Longer implants ª Improved biomechanics ª Eliminates the need for sinus augmenta1on
85. Pterygoid implants If fully guided surgery is used, abutments can be chosen or milled prior to surgical placement
86. Pterygoid implants ª Implants placed with the aid of a surgical template ª Semi-‐guided surgical placement was employed
87. Pterygoid implants ª Combina1on of 1lted implant and a pterygoid implant ª Eliminates the need for sinus augmenta1on ª Occlusion is anterior guidance
88. Zygoma1c implants ª Introduced by Branemark in the late 1980’s ª Pa1ents with moderately resorbed maxillae ª Designed to be used in concert with 2-‐4 implants placed in the anterior maxilla ª Success rates have been very high in conven1onal pa1ents (Branemark, 2004; Aparicio et al, 2006; Bedrossian et al, 2006; Kahnberg et al, 2007; Bedrossian et al, 2012).
89. Zygoma1c implants Complica1ons – rare but significant ª Oral antral fistula ª Postopera1ve maxillary sinusi1s ª Peri-‐orbital hematoma ª Facial swelling ª Penetra1on of the orbit
90. Zygoma1c implants No longer recommended for pa1ents with an intact palate ª Distor1on of palatal contours Other op1ons available that are more effec1ve. ª Tilted implants ª Pterygoid implants ª Sinus augmenta1on
91. Zygoma1c implants ª Pa1ent was allergic to acrylic resin ª Zygoma1c implants used to avoid sinus augmenta1on ª Zygoma1c implants did not alter the contours of the restora1on or impair the tongue space
92. Zygoma1c implants Used for pa1ents with major defects of the hard palate ª Useful for incomplete repaired cleV lip and palate pa1ents ª Edentulous maxillectomy pa1ents with large defects ª Success rates have been good (Schmidt et al, 2004; Schmidt, 2007) Courtesy A. Sharma
93. Zygoma1c implants Issues ª Radia1on effects ª Hygiene access ª Long term survivabilty Best suited for total palatectomy defects Courtesy A. Sharma
94. Zygoma1c implants Prosthodon1c issues ª Two implants per side ª Splint all implants together ª Implant supported vs implant assisted design depends on implant distribu1on pa^ern Best suited for total palatectomy defects Courtesy A. Sharma
95. v Visit ffofr.org for hundreds of addi1onal lectures on Complete Dentures, Fixed Prosthodon1cs Implant Den1stry, Removable Par1al Dentures, Esthe1c Den1stry and Maxillofacial Prosthe1cs. v The lectures are free. v Our objec1ve is to create the best and most comprehensive online programs of instruc1on in Prosthodon1cs


 Computer Guided Treatment Planning and Surgery
Computer Guided Treatment Planning and Surgery
 Single Tooth Defects in Posterior Quadrants
Single Tooth Defects in Posterior Quadrants
 Angled Implants
Angled Implants
 Implants and RPDs
Implants and RPDs
