Transcript of “Dental Implants – Cement Retention vs Screw Retention”
1. Dental Implants Cement retention vs screw retention John Beumer III DDS, MS Robert Faulkner DDS, MS Division of Advanced Prosthodontics, UCLA This program of instruc1on is protected by copyright ©. No por1on of this program of instruc1on may be reproduced, recorded or transferred by any means electronic, digital, photographic, mechanical etc., or by any informa1on storage or retrieval system, without prior permission.
2. Cement vs screw reten1on Which method is preferred to retain implant prostheses? Both methods can be employed if used properly.
3. Cement retained prostheses Advantages – Simplicity – Familiarity – Idealize occlusal contacts • Occlusal contacts are not effected by the screw access channel – Esthe1cs – • Porcelain occlusal surfaces can be developed – Reduces risk of porcelain chipping and fractures associated with the screw access channel Cement retained prosthesis Screw retained prosthesis
4. Cement retained prostheses Disadvantages and concerns ª Requires precise margin placement ª Requires a me1culous technique ª The volume of cement used must be carefully controlled ª Cements becomes aOached to the machined surface of abutment of the micro-‐rough surface of the implant difficult to remove ª Prosthesis is not easily retrieved ª Recurrent loss of reten1on when reten1on and resistance form of the abutment is subop1mal Residual cement may be impacted subgingivally secondary to incomplete sea1ng of the crown or extrusion of cement subgingivally predisposing to: ª Peri-‐implant mucosi1s ª Peri-‐implan11s
5. Major Problem Sub-‐gingival reten1on of cement Two issues: ª Impac1on of cement subgingivally during cementa1on ª Incomplete sea1ng of the crown These two phenomenon predispose to peri-‐implan**s – An inflammatory process affec1ng the 1ssues around an osseointegrated implant in func1on, accompanied by bone loss. Courtesy Dr. C. Goodacre
6. Major Problem Sub-‐gingival reten1on of cement Two issues: ª Impac1on of cement subgingivally during cementa1on ª Incomplete sea1ng of the crown It may take several years before the excess cement becomes apparent (Thomas, 2009) Courtesy Dr. C. Goodacre
7. Major Problem – Retained cement ª If the margin is sub-‐gingival, there will be residual cement 100% of the 1me (Linkevicius et al, 2013). ª Peri-‐implan11s may ensue, leading to loss of implants and o`en the adjacent teeth (Wilson, 2009; Wadhani, et al, 2011). ª 80% of cases of peri-‐implan11s are secondary to sub-‐gingival cement accumula1ons (Wilson, 2009) ª
8. Courtesy of Dr. C. Wadhwani These pa1ents presented with peri-‐implan11s ª The implants are s1ll anchored in bone but their prognosis is poor ª Note cement adherent to the surfaces of the implants ª The methods for decontamina1on of the implant surfaces and gra`ing these site have been problema1c Major Problem – Retained cement Courtesy of Dr. G. Perri
9. If the cement margin is subgingival it is not possible to remove all the cement (Linkevicius et al, 2013) Case report Prepable abutment An impression was obtained with an impression coping and the prepable abutment was aOached to the fixture analogue imbedded in the master cast. Courtesy Dr. S. Parvispour
10. Subgingival cement accumula1on Prepable abutment ª The abutment was prepared so that the margin is slightly sub gingival. ª The metal ceramic crown was completed in a customary fashion. ª The abutment was secured to the implant fixture and the crown is then cemented. Courtesy Dr. S. Parvispour Case report
11. Subgingival cement accumula1on Prepable abutment v The pa1ent was unhappy with the esthe1c result and so a hole was drilled into the occlusal surface in order to access the abutment screw. The crown and abutment was then removed v Note the accumula1on of cement subgingivally. Courtesy Dr. S. Parvispour Case report
12. Sub-‐gingival cement accumula1on Implant Surface Bone Epithelium Sulcus Circumferen1al collagen fibers ª Peri-‐implant 1ssues are more easily displaced from the surface of the implant because of the absence of a connec1ve fibers aOached to the implant. ª As a result the epithelial aOachment is easily severed and cement can be impacted to the level of the bone and on to the surface of the implant. Why is there a greater risk of cement accumula1on in the sulcus of implant crowns?
13. Challenges of cementa1on ª Removal of cement is extremely difficult, especially when it is adherent to the micro-‐rough surface of the implant. ª In this pa1ent it led to the failure of the implant and compromised the periodontal support for the adjacent teeth Courtesy C. Wadhani
14. Challenges of cementa1on TPS (titanium plasma spMachined Machined c.p. Ti Acid etched micro-‐rough implant surface Machined surface of abutment When cement becomes adherent to either the surface of a machined or milled abutment or the micro-‐rough surface of the implant, it is very difficult and some1mes impossible remove. Anodized implant surface
15. If you insist upon cementa1on ª Control the volume of cement ª Avoid the use of prefabricated abutments ª Use customized abutments with supra-‐gingival margins in the posterior quadrants, especially when there are significant undercuts and concavi1es associated with the abutment ª Idealize reten1on and resistance form ª Avoid the use of prefabricated abutments Cement retained prostheses
16. Preparing custom abutments for cementa1on ª The por1on engaging the crown should not be polished. It can be roughened or prepared with grooves. ª The por1on adjacent to the gingival 1ssues should be highly polished
17. Types of cements used v Polycarboxylate cements should not be used because they contain fluoride which will corrode the 1tanium surface of the implant or abutment. v Resin cements, containing hydroxylated ethymethacrylate, (HEMA) which is potent cytotoxic agent, should be avoided. v Zinc oxide and eugenol cements are favored. They are an1-‐bacterial and are radio-‐opaque. Courtesy Dr. C. Goodacre
18. Types of cements recommended Zinc oxide and eugenol cements are favored ª They possess an1bacterial proper1es ª They are radio-‐opaque (However, excess cement on the buccal and labial surfaces may not be seen) Courtesy Dr. C. Goodacre
19. Cementa1on Recommenda1ons Use a provisional cement (ZOE) such as temp-‐bond unless the reten1on is compromised by a short abutment, a very tapered abutment, or the screw access hole eliminates reten1ve surface(s)
20. Cementa1on Recommenda1ons When reten1on is compromised by implant angula1on and the posi1on of the abutment screw orifice, use zinc phosphate cement Courtesy of Dr. C. Goodacre
21. Cementa1on Recommenda1ons This implant crown loosened a`er 2 months when cemented with ZOE. Courtesy of Dr. C. Goodacre
22. Poor reten1on and resistance form secondary to excessive labial inclina1on When reten1on is compromised by the angula1on of the abutment screw channel, another op1on is to retain the crown with a lingual cross pinning screw.
23. Problem -‐ Insufficient interocclusal space to design an abutment with appropriate resistance and reten1on form. ª Recurrent loss of reten1on is seen most o`en when lack of interocclusal space prevents development of custom abutments with sufficient axial wall lengths to retain the crown. ª Another advantage with screw reten1on -‐ the emergence profile of the crown is idealized Courtesy G. Perri Screw reten1on favored when there is Lack of interocclusal space
24. This custom abutment has an excessive taper. Cementa1on Recommenda1ons Custom abutments must be designed with appropriate reten1on and resistance form
25. The addi1on of grooves will improve resistance form and is recommended for single tooth molar restora1ons. Cementa1on Recommenda1ons Custom abutments must be designed with appropriate reten1on and resistance form
26. Cementa1on procedures Carefully control the volume of cement used (Wadhwani and Pineyro (2009) ª The intaglio surfaces of the crown/s is lined with teflon tape ª The implant restora1on is seated firmly onto the abutments and then removed ª A fast seing vinyl polysiloxane material is injected into the intaglio surfaces of the crown/s. ª The excess material is used as a handle. When the material has polymerized, it is removed from the crown/s.
27. Carefully control the volume of cement used (Wadhwani and Pineyro (2009) ª The teflon tape is removed from the crown/s ª A suitable cement is prepared and a thin layer is placed inside the crown/s ª The VPS abutment analogues are seated into posi1on and the excess cement is removed. ª A very thin layer is added and the crown is seated into posi1on ª Excess cement is removed with curved plas1c instruments. Cementa1on procedures
28. Challenges of cementa1on Plakorm reduc1on (plakorm switching) ª If the cement becomes impacted below the margin, its removal is problema1c ª Access is extremely difficult if not impossible without laying a so` 1ssue flap Courtesy Dr. G. Perri
29. Challenges of cementa1on ª How will you remove the cement if it becomes impacted beneath the margins of this implant crown? ª More than likely, you will not, given the severity of the undercut associated with the custom abutment. ª Therefore, under these circumstances it is advisable to place the margins supra-‐gingival.
30. Cement retained prostheses Posterior quadrants It is advisable that margins of custom abutments be designed to be slightly supra-‐ gingival in order to facilitate removal the cement
31. Cement retained prostheses • Ven1ng is not effec1ve Ven1ng makes it easier to seat the crowns, especially a mul1-‐unit implant born prosthesis, but does not prevent impac1on of cement sub-‐gingivally.
32. Cement retained prostheses Packing retrac1on cord is ineffec1ve in preven1ng subgingival cement accumula1ons ª There is risk of detaching the epithelial aOachment when packing the cord ª Sub-‐gingival cement accumula1on is not prevented by packing gingival retrac1on cord prior to cementa1on ª Cement has been shown to extrude apical to the retrac1on cord (Wadhwani et al, 2011).
33. Avoid the use of preformed non-‐prepable abutments Issues of concern v Posi1on of the cement margin in rela1on to the gingival margin v Par1cularly significant in the anterior region v Impac1on of cement into the gingival sulcus is highly likely v Difficulty in sea1ng the crown because of hydraulic pressure
34. Preformed abutments are problema1c v The margin between the crown and the abutment does not follow the gingival margin. v There is significant risk of trapping cement beneath the gingival 1ssues upon cementa1on in the proximal areas. Courtesy Dr. A. Pozzi
35. Preformed nonprepable abutments ª This implant crown was retained by a prefabricated abutment. ª Note the inflammation associated with the peri-implant gingiva 2 1/2 years post insertion. ª Radiograph revealed significant bone loss. Dx – Peri-‐implan11s
36. Preformed nonpreparable abutments This pa1ent presented with peri-‐implant mucosi1s 3 years post inser1on of the crown. The initial x-ray appeared to indicate that the crown was seated. A subsequent x-ray, taken at right angles to the long axis of the implant, revealed that the crown, was not seated. • Inability to completely seat the crown onto the abutment is a common complication associated with preformed abutments. • Lingual access holes may help relieve the hydraulic pressure and enable seating of the crown but it will not be possible to remove all the cement that extrudes subgingivally
37. Apical migra1on of bone and peri-‐implant so` 1ssues in the esthe1c zone Causes of apical migra1on of bone and so` 1ssues • Thin layer of labial bone overlying the implant upon implant placement (less than 1 mm) • Poor surgical technique • Peri-‐implan11s • Natural progression Even when implants are placed properly and in ideal posi1on and with proper angula1on, there is risk of apical migra1on long term, even in a pa1ent with good oral hygiene
38. Apical migra1on of bone and peri-‐implant 1ssues • Thin labial bone • Labial inclina1on • Poor surgical technique • Peri-‐implan11s Even when implants are placed properly and in ideal posi1on and with proper angula1on, there is risk of apical migra1on long term, even in a pa1ent with good oral hygiene This a concern in the esthe1c zone
39. Avoiding subgingival cement accumula1on in the esthe1c zone Implant crowns with supra-‐gingival margins – Fabricate the custom abutment/s with a ceramo-‐metal – Bake porcelain onto the custom abutment with margin placed supra-‐gingivally
40. Cement the crown to an abutment outside the mouth and retain it with the abutment screw • In the esthe1c zone this technique requires that the abutment screw exit in the cingulum area.
41. ª Retrievability ª Avoid trapping cement subgingivally ª Less risk of peri-‐implan11s ª Carry restora1on more subgingivally ª For more ideal emergence profile and contour. ª Advantageous in the esthe1c zone ª More predictable sea1ng a bridge with a pon1c ª Predictable reten1on par1cularly when a cemented restora1on would have a very short axial wall because of limited inter-‐occlusal or restora1ve space. Arguments in favor Screw reten1on
42. In the esthe1c zone screw reten1on is preferred Advantages ª Retrievability ª Less risk of peri-‐implan11s ª Extend the porcelain margins deeper subgingivally ª Apical migra1on will not compromise the esthe1cs of the prosthesis
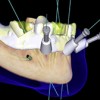
43. UCLA abutment technique The restora1on is connected directly to the implant plakorm
44. UCLA abutment technique Advantages ª Retrievability ª Less risk of peri-‐implan11s ª Extend the porcelain margins deeper subgingivally ª Accounts for apical migra1on of bone and peri-‐implant so` 1ssues
45. Custom substructures and abutments with reten1on provided by cross linking screws Advantages ª Retrievability ª Less risk of peri-‐implan11s ª Extend the porcelain margins deeper subgingivally ª Accounts for apical migra1on of bone and peri-‐implant so` 1ssues Screw reten1on
46. Custom substructures and abutments with reten1on provided by cross linking screws Advantages ª Retrievability ª Less risk of peri-‐implan11s ª Extend the porcelain margins deeper subgingivally ª Accounts for apical migra1on of bone and peri-‐implant so` 1ssues Screw reten1on
47. v Visit ffofr.org for hundreds of addi1onal lectures on Complete Dentures, Fixed Prosthodon1cs Implant Den1stry, Removable Par1al Dentures, Esthe1c Den1stry and Maxillofacial Prosthe1cs. v The lectures are free. v Our objec1ve is to create the best and most comprehensive online programs of instruc1on in Prosthodon1cs


 Angled Implants
Angled Implants
 Prosthodontic Procedures and Complications
Prosthodontic Procedures and Complications
 Single Tooth Defects in Posterior Quadrants
Single Tooth Defects in Posterior Quadrants
 Computer Guided Treatment Planning and Surgery
Computer Guided Treatment Planning and Surgery
