The delivery appointment is the process of eliminating errors. The objective this appointment is to perfect the adaptation of the dentures and to make the necessary adjustments to obtain perfect harmony in occlusion. Pressure indicating paste is used to perfect adaptation, disclosing wax is used to adjust the denture borders, and clinical remount records are used to refine the occlusion. This program describes and illustrates these procedures in detail.
Complete Dentures» Next Lecture› [next_page]
Complete Dentures – Insertion and Followup — Course Transcript
- 1. 30. Insertion and Followup John Beumer III, DDS, MS and Robert Duell DDS Division of Advanced Prosthodontics, Biomaterials and Hospital Dentistry UCLA School of Dentistry This program of instruction is protected by copyright ©. No portion of this program of instruction may be reproduced, recorded or transferred by any means electronic, digital, photographic, mechanical etc., or by any information storage or retrieval system, without prior permission.
- 2. Insertion Appointment In order to successfully complete this appointment, you will need the polished dentures, the articulator with the maxillary remount cast mounted and the mandibular remount cast.
- 3. Reexamine the tissue side of the dentures and carefully remove any bubbles present with a Kingsley scraper or other sharp instrument. Insertion Appointment Prior to delivery the dentures must be soaked in water for 72 hours.
- 4. Insertion Appointment Sequence* Adjust denture base Adjust denture borders Remount in centric relation Equilibrate in lateral excursion Patient education * Prior to the insertion appointment the old dentures must be left out of the mouth for 24 hours.
- 5. “ The insertion appointment is the process of eliminating errors.” F. J. Kratochvil, 1966 Purpose – Insertion Appointment Faithfully executing the steps of the insertion appointment will save time and money.
- 6. Adjusting the Denture Base Zinc oxide paste is used as a pressure indicating paste (PIP) to detect improper adaptation. Here, it has been placed into a disposable syringe for easy use. The PIP spray is used in patients with xerostomia in order to prevent the PIP from sticking to the mucosa.
- 7. Adjusting the Denture Base PIP Sequence Dry denture surface Brush a thin even layer of PIP onto the surface of the denture Seat the denture with pressure in the first molar region Remove immediately Inspect and adjust bearing surface as necessary
- 8. The PIP pattern indicates severe pressure on the portion of the denture that overlies the torus. Adjusting the Denture Base
- 9. This area is adjusted with an acrylic burr. When completed the brush marks are mostly absent and the posterior palatal seal bead is showing. Adjusting the Denture Base
- 10. PIP the mandibular denture Use smooth even brush strokes Carefully insert denture so as to avoid wiping off PIP in undercut areas Adjust as necessary Adjusting the Denture Base Pay particular attention to the mylohyoid ridge region.
- 11. Note the areas of excessive tissue pressure on the labial and buccal slopes of the ridge. These are carefully adjusted with an acrylic burr . Adjusting the Denture Base When completed with this procedure most of the brush marks should be obliterated and there should no areas of tissue displacement noted.
- 12. Adjusting the Denture Borders Temper the wax in the syringe in a water bath. Apply disclosing wax to the dried denture border. Carefully insert the denture and mold the borders of the selected area. Disclosing wax is used to check the length of the denture borders. In this example it has been placed in a disposable syringe.
- 13. Carefully adjust the denture flange as necessary. Reapply, border mold and adjust until areas of overextension are eliminated. Adjusting the Denture Borders
- 14. Other examples of commonly overextended areas These flanges are too thick These flanges are too long Adjusting the Denture Borders
- 15. Clinical Remount Adjusted denture bases seat more accurately than record bases Accommodate for errors made during the making of centric relation records “ Measure twice, cut once ” Purpose To Correct for the fact that :
- 16. Clinical Remount Seat the posterior palatal seal Place two cotton rolls between the posterior teeth and have the patient bite down for 5 minutes.
- 17. The maxillary denture has already been mounted on the articulator with the plaster remount cast and maxillary facebow transfer jig. Clinical Remount –Lingualized Occlusion
- 18. Place compound sticks in the water bath at 105 degrees. Make sure you use enough compound to cover the posterior teeth. Apply the melted compound to the occlusal surfaces of the posterior teeth. Clinical Remount – Lingualized Occlusion
- 19. Carry to mouth and have the patient close in centric relation just short of tooth contact. While making the record, instruct the patient to retrude and elevate the tongue. This will ensure that the condyles are properly seated while making the record. Clinical Remount – Lingualized Occlusion Make centric relation record and prove the record
- 20. Remove the record. Chill in cold water and trim so that only the cusp tip indentations remain. Trim the buccal side so that the seating of the dentures can be visually checked. Clinical Remount – Lingualized Occlusion
- 21. Return the record to the mouth and recheck the record. Contact should be equal and simultaneous bilaterally. If not repeat the record. Observe the maxillary denture as the patient closes. If the denture moves during closure repeat the record . Clinical Remount – Lingualized Occlusion
- 22. Clinical Remount – Lingualized Occlusion Using the remount casts the dentures are remounted on the articulator. Make sure to lock the condyles in centric while remounting the dentures.
- 23. Clinical Remount – Lingualized Occlusion Begin by equilibrating in centric relation. If your original Centric Relation record was correct, little or no adjustment will be necessary.
- 24. Make a protrusive record. Instruct the patient to bring their mandible forward 8-10 mm when making the record. Clinical Remount – Lingualized Occlusion
- 25. Clinical Remount – Lingualized Occlusion Protrusive record Transfer the record to the articulator and insert one of the protrusive inserts. Hold the upper member of the articulator down into the record and adjust the condylar inclination.
- 26. Clinical Remount – Lingualized Occlusion Protrusive record A steeper insert (30 degrees) was eventually chosen. The dentures are seated in the protrusive record and the condylar shaft is in contact with the protrusive insert. We are now ready, if necessary, to equilibrate in excursions .
- 27. Check excursions. This is protrusive. If necessary, adjust the occlusion to restore bilateral balance. Clinical Remount – Lingualized Occlusion
- 28. Clinical Remount – Lingualized Occlusion Bilateral balance in lateral excursions is the desired outcome. Working Balancing Centric
- 29. Good esthetics Freedom of non-anatomic teeth Potential for bilateral balance Centralizes vertical forces Minimizes tipping forces Facilitates bolus penetration (mortar and pestle effect) Lingualized Occlusion High esthetic demands Severe mandibular ridge atrophy Displaceable supporting tissues Malocclusion Previous successful denture with Lingualized Occlusion Indications for use Advantages
- 30. Clinical Remount – Monoplane Occlusion Use a centric relation record and the remount cast to mount lower.
- 31. Clinical Remount – Monoplane Occlusion Equilibrate in centric first. Neutrocentric
- 32. Clinical Remount – Monoplane Occlusion Neutrocentric When complete all of the maxillary and mandibular posterior teeth plus the central incisors will be on the occlusal plane.
- 33. Clinical Remount – Monoplane Occlusion Monoplane with balancing ramps Equilibrate in centric as before. Balancing ramp is incorporated into the denture base .
- 34. Clinical Remount – Monoplane Occlusion Monoplane with balancing ramps Equilibrate in working, balancing and protrusive. Upon completion the articulator should slide easily from working to balancing to protrusive and back. There should be no bumps along the road. If the contacts on the balancing ramps are insufficient they may be supplemented with autopolymerizing acrylic resin. Balancing Protrusive Working
- 35. Patient Management Explain the following to the patient Limitation of the dentures Expected tissue response Care of the prostheses and tissues Desirable followup treatment Leave out the dentures at night * Remember the kind of patient with whom you are dealing.
- 36. House Classification of Patients Philosophical – Rational, sensible, organized and overcomes conflicts (Expectations are real) Exacting – Methodical, precise and accurate; places severe demands (Must reach an understanding before starting treatment) Indifferent – Apathetic, uninterested, uncooperative and lacks motivation; blames dentist for poor health; pays no attention to instructions (Unfavorable prognosis) Hysterical – Emotionally unstable, excitable, apprehensive (Psychiatric help may be required)
- 37. 24 hour check Inquire about the patient’s problems and conduct a thorough oral examination Check the denture for pressure areas and adjust the denture as needed with PIP Check borders for overextension with disclosing wax and adjust as needed Evaluate occlusion, refine equilibration as necessary, and recheck finish and polish .
- 38. Ask the patient where their worst sore is. 24 hour check
- 39. 24 hour check Note the ulcer associated with the denture border overlying the canine eminence.
- 40. Note the posterior palatal seal area: The bead is too deep and too sharp. Note the ulcer at the midline. 24 hour check
- 41. 24 hour check Note the lesions associated with the anterior mandibular denture border. They correspond to the PIP pattern .
- 42. 24 hour check This area represents a bony spicule just beneath the mucosa. Unless the denture is properly adjusted in this area, the irritation will progress to ulceration.
- 43. 24 hour check Inspect the frenum areas. This is the anterior maxillary frenum. It is the most common frenum to become irritated from denture overextension.
- 44. With the aid of disclosing wax, the frenum area is adjusted with the small diameter acrylic burr using a slow speed handpiece . 24 hour check
- 45. Beware of the inferior alveolar nerve 24 hour check In patients with severe resorption of the alveolar ridge, a portion of the inferior alveolar nerve may be exposed. Pressure in these areas may cause significant pain.
- 46. Evaluate the Occlusion If you observe change repeat the clinical remount procedure Open contact
- 47. Neuromuscular control may be the single most significant factor in the successful manipulation of complete dentures under function Complete Denture Manipulation Tongue function and denture wearing experience are important prognostic indicators.
- 48. Common Problems Mandibular denture Discomfort Poor retention and stability Lack of support Maxillary denture Poor retention and stability Esthetics and phonetics
- 49. Discomfort May be Secondary to: Open vertical dimension of occlusion Inaccurate centric relation record Lack of occlusal balance Poor denture base adaptation Inappropriate denture base extensions
- 50. Retention and Stability Compromised by: Occlusal discrepancies Poor denture base adaptation Inadequate denture extensions These factors are controlled by the dentist
- 51. Retention and Stability also Affected by: Moderate to severe resorption Unfavorable floor of mouth posture Retruded tongue position Reduced salivary flow Poor neuromuscular control These factors are beyond the control of the dentist
- 52. Possible Solutions Osseointegrated implants Denture Adhesives Permanent soft liners
- 53. Result: a. Improved retention. Note denture snaps onto retention bar. b. Improved stability (from the implants and the retention bar). c. Improved support (anteriorly). d. Better control of the bolus (tongue no longer must position denture and control bolus simultaneously and can concentrate on control of the bolus). Possible Solutions 1. Dentures retained with osseointegrated implants
- 54. Possible Solutions Denture adhesives Powder Cream Pads We generally discourage the use of denture adhesive. In very few cases for short periods of time adhesive may help keep new dentures in place. Denture retention, particularly in the mandible, is a matter of neuromuscular control which is gained by practice and time.
- 55. Possible Solutions Indications Limited to mandibular dentures Chronic soreness Bruxers No attached gingiva Contraindications Poor oral hygiene Patients with xerostomia Must be replaced more frequently Permanent soft liners – Silicone elastomers
- 56. Moloplast-B Poor ridge height Lack of attached mucosa Special burs required for adjustment Possible Solutions
- 57. Check the thickness of the maxillary palatal portion. A common problem is excessive thickness. Reevaluate the position of the maxillary anterior teeth. If everything appears normal it may be a matter of time for the patient to adapt. Open vertical dimension of occlusion Problems with Phonetics
- 58. Complaints with Esthetics Allow the patient to wear the denture for a period of time. If the patient is unhappy with their appearance occasionally the anterior teeth must be changed.
- 59. Gagging Palate excessively thick Palatal extension too long Lack of tongue space (teeth set too far to the lingual


 Implants and RPDs
Implants and RPDs
 Cement Retention vs Screw Retention
Cement Retention vs Screw Retention
 Single Tooth Defects in Posterior Quadrants
Single Tooth Defects in Posterior Quadrants
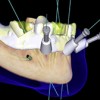 Computer Guided Treatment Planning and Surgery
Computer Guided Treatment Planning and Surgery
