Facial defects result from trauma, treatment of neoplastic disease or congenital disease. Oncologic defects are restored prosthetically. The retention provided by these implants allows for the use of large prostheses on movable tissues because the margins can be made thinner and more flexible. Acceptance by patients is significantly enhanced because of the quality of retention, the improved esthetics that results from accurate and repeatable positioning of the prosthesis and the ease of maintenance. This program discusses the types of tumors that lead to these defects and the basic principles of designing and fabricating facial prostheses.
Maxillofacial Prosthetics – Restoration of Facial Defects – Etiology and Basic Priniciples — Course Transcript
- 1. Restoration of Facial Defects Etiology and Basic Principles John Beumer III DDS, MSDivision of Advanced Prosthodontics, Biomaterials and Hospital Dentistry UCLA School of Dentistry*The material in this program of instruction is protected by copyright ©. Nopart of this program of instruction may be reproduced, recorded, ortransmitted by any means, electronic,digital, photographic, mechanical, etc.or by any information storage or retrieval system, without prior permission.
- 2. Restoration of Facial DefectsA difficult challenge. Both surgical reconstruction andprosthetic rehabilitation have distinct limitationsv The surgeon is limited by the complexity of the structures to be reconstructed, the availability of tissue, compromise of the local vascular bed by radiation in tumor patients and the need for visual inspection of oncologic defectsv The prosthodontist is limited by the properties of the materials available, mobility of the tissues adjacent to the defects and difficulty of establishing adequate retention for large combination facial prostheses.
- 3. Table of Contentsv Etiology of facial defectsv Presurgical consultationv Surgical reconstruction vs prosthetic rehabilitationv Materialsv Alterations at surgery to enhance the prosthetic prognosis v Nasal defects v Orbital defects v Auricular defects v Large midfacial defectsv Basic principles v Form and symmetry v Surface texture v Lines of juncture v Coloration
- 4. Etiologyv Facial neoplasms v Basal cell carcinoma v Squamous carcinoma v Malignant melanomav Craniofacial anomalies v Microtiav Trauma v Self inflicted gunshot wounds
- 5. Facial NeoplasmsBasal cell carcinoma v Benign v Chronic immunosuppression dramatically increases the rate (Berg and Otley, 2002; Euvrad et al, 2003; Hasegawa et al, 2005). v Locally destructive when unattended v Clinical presentations: v Small nodular lesions with a central ulcer often covered with a crusted core
- 6. Basal cell carcinomav Treatmentv Surgical excisionv Mohs’ chemosurgery (Mohs, 1976; Nelson et al, 1997)v Radiation v 45-60 Gy
- 7. Facial Neoplasms Basal cell carcinomaLarge defects result when:v Tumors are left untreated for a number yearsv Extensive recurrences
- 8. Facial NeoplasmsLarge extensive basal cell carcinoma
- 9. Facial NeoplasmsThese recurrent basal cell carcinomas extended far beyond their original sites and required aggressive re- resections resulting in large facial defects.
- 10. Facial Neoplasms Basal Cell CarcinomasThese recurrent basal cell carcinomas extended farbeyond their original sites and required aggressive re-resections resulting in large facial defects.
- 11. Facial Neoplasms – Basal cell carcinoma Radiation therapyBefore After In large tumors such as this one that have invaded cartilage, only about 30% fail and require surgery
- 12. Basal cell carcinoma Radiation Therapy Patient developed aPostradiation – Note recurrence severaldestruction of local years later requiringstructures extensive resection
- 13. Basal cell carcinomaMohs’ chemosurgery v A tissue fixative is applied to the tumor volume v These tissues are then removed surgically and the specimen is tagged v The specimen is imbedded, sectioned and immediately examined microscopically v Persistent tumor is identified, its location confirmed and these tissue areas are re-resected on the patient until the specimens are tumor free. v The defects created are irregular and often residual facial structures such as portion of the nose remain
- 14. Basal cell carcinomaMohs’ chemosurgery These defects are more challenging to restore prosthodontically because: v The defect tissues are not lined with skin grafts. This makes it difficult to engage the defect so as to enhance retention and the stability of the prosthesis v Residual facial structures are often displaced making it difficult to restore the appearance of size and symmetry of the lost facial structures
- 15. Facial neoplasmsMalignant v Usually well differentiated v Can be locally destructive v Advanced tumors can spread to the regional nodes v Squamous carcinomas associated with chronic immunosuppression and organ transplantation behave more
- 16. Facial neoplasms Squamous carcinomaTreatment v Surgery v Radiation therapy
- 17. Facial neoplasms Squamous carcinomaThis tumor has been present for many yearsand has destroyed much local tissue
- 18. Carcinomas arising from the nasal septum These tumors are usually discovered late and require large resections of the nose, upper lip and the maxilla.
- 19. Facial neoplasms Malignant melanomaThese tumors require aggressive surgical excision.
- 20. Congenital anomaliesMicrotia Implant retained auricular prostheses have become a viable option. Why? v High levels of implant predictability (Parel and Tjellstrom, 1991; Jacobsson et al, 1992; Sugar and Beumer, 1994; Roumanas et al, 2002). v Consistently excellent esthetic results v Fewer and less invasive surgical procedures v Reduced cost as compared with surgical reconstruction
- 21. Traumal Self inflicted gunshot wounds
- 22. Mucormycosis and aspergillosisThis patient required removal of the orbital contents tocontrol the infection resulting in facial disfigurement.
- 23. Surgical reconstruction vs prosthetic restoration of large facial defectsv Many patients prefer that their defects be masked with their own tissues rather than with a prosthesisv Not all patients can accept an artificial facial prosthesisv Surgical reconstruction is preferred with small nasal defects.v Acceptable results have been achieved by some surgeons with staged reconstruction of congenital ear defects (Brent, 2002)The tip and left ala have been surgically reconstructed inthis patient.
- 24. Surgical reconstruction vs prosthetic restoration of large facial defects Reconstruction of total rhinectomy defects is extremely difficult with current techniques and the results are unpredictable
- 25. Surgical reconstruction vs prosthetic restoration of large facial defectsPerceptions have changedregarding facial prosthesesv Improvements in materials used in facial prostheticsv Facial prostheses achieve superior esthetic resultsv Implant retained facial prostheses have achieved wide acceptance among surgeons, prosthodontists and patients (Flood et al, 1998; Markt et al, 2001;Chang et al 2005) Prosthesis for a total rhinectomy defect
- 26. Patient acceptance – Implant retained facial prosthesesImproved because: v Quality of the retention v Improved esthetics that result from accurate and repeatable positioning v Thinner margins possible to better accommodate mobile tissues v Ease of maintenance
- 27. Surgical reconstruction vs prosthetic restoration of large facial defectsProsthetic restorations are favored v When recurrence of tumor is likely v Because of the need to monitor surgical site for recurrence v With large defects – Reconstruction of large defects is difficult, time consuming and technically difficult and the outcomes are unpredictable v When the defect tissues are heavily irradiated
- 28. Presurgical ConsultationIssues v Psychosocial v Impressions v Photographs v Explain the limits of the prosthetic rehabilitation v Brief review of prosthetic care procedures
- 29. Presurgical ConsultationPsychosocial issues v Challenges confronting patients v Mortality v Morbidity v Functional impairments v Esthetics v Quality of life – Social function v Challenges confronting the provider v Establish lines of communication v Maintain empathy and compassion while at the same time maintaining the ability to motivate the patient to perform needed home care procedures
- 30. Presurgical ConsultationPsychosocial issuesv Family members or significant others may be important assets in communicating needed information to the patients. v Because these initial consultations are often conducted under stressful conditions (the patient has frequently jus been informed of the diagnosis and treatment) patients frequently do not absorb all the information delivered by the prosthodontist.v When the patient and/or their families are having difficulty understanding the challenges and their responsibilities for home care referral to a clinical psychologist or social worker is advised.
- 31. Presurgical Consultationv Impressionsv Photographsv Explain the benefits and limits of prosthetic rehabilitation v Esthetics – Prostheses in movable tissues v Limits of the physical properties of facial materials v Retention – Skin adhesives vs Implantsv Brief review of prosthetic care procedures
- 32. Materials used for facials prostheses Ideal biologic properties of processed facial materials v The cured and any released materials should not irritate the supporting tissues v The cured and any released materials should be non-allergenic v The cured and any released materials should be nontoxic
- 33. Materials used for facials prosthesesv Ideal physical and mechanical properties of processed facial materials v The cured material should not transfer heat or cold to supporting tissues v The cured material should be resistant to abrasion v The cured material should be light weight v The cured material should have high tensile strength v The cured material should have low surface tension and low water sorption to resist staining v The cured material should not be dissolved by solvents, primers or adhesives v The cured material should be odorless v The cured material should not support the growth of micro- organisms
- 34. Materials used for facials prosthesesv Ideal physical and mechanical properties of processed facial materials v The cured material should be chemically inert v The cured material should be cleansable with common disinfectants without loss of detail at the surface or margins v The cured material should be dimensionally stable v The cured materials’ flexibility should mimic that of the tissues it replaces v The cured material should be stable at a range of temperatures v Thin feather edges of the material should not tear v The material should be inexpensive v The material should have lifelike translucency
- 35. Materials used for facials prostheses v Methyl methacrylate v Polyurethanes v Silicones
- 36. Methyl methacrylate Developed in the 1930’s Desirable properties v Color stable v Easy to color v Easy to process v Margins can be feathered v Excellent cosmetic results Undesirable properties v Rigidity v The material transfers heat or cold to supporting tissues
- 37. Polyurethane elastomers Desirable properties v Excellent edge strength v Margins can be feathered v Elasticity v Colorability v Excellent cosmetic results Undesirable properties v Not color stable when exposed to ultraviolet light secondary to surface oxidation v Limited life span (3-6 months) v Difficult to process particularly under humid conditions v Poor compatibility with adhesive systems
- 38. Silicone elastomers* Desirable properties v Color Stable v Easy to process v Colorability v Reasonable edge strength v Margins can be feathered v Color stable when exposed to ultraviolet light v Lifespan – 1-3 years Undesirable properties v Lack of flexibility v Extrinsic coloration tends to wear off*A detailed discussion of the silicone elastomers can befound in Powers J and Kiat-annuay. ”Materials” inRehabilitation of Facial Defects (Ch 5) in MaxillofacialRehabiliation 3rd edition. Eds Beumer J, Marunick Mand Esposito S. Quintessence Publishing Co. Chicago,Ill 2011. pgs. 260-71
- 39. Materials used for facial prosthesesCommon problems To date, none of the commercial materials satisfy all the requirements of the ideal material. Each of the materials available has its strengths and weaknesses. Even though each type of maxillofacial elastomer has its own unique physical and mechanical properties, they all share a few common clinical problems which can be grouped into two categories. v Discoloration of the prosthesis over time v Degradation of static and dynamic mechanical properties of the polymeric materials.
- 40. Materials used for facials prosthesesFuture research should concentrate on several major goals:v Improvement of the physical and mechanical properties of existing materials available or development of new alternative materials so that replacement materials will behave more like human tissue and increase the service life of the prosthesisv Identification of color stable coloring agents for coloring facial prostheses that are compatible with different types of elastomersv Development of a scientific method of color matching to human skinv Development of a scientific color formulation system that conforms to the color matching tool to objectively replicate human skin shades
- 41. Alterations at Surgery to Enhance the Prosthetic Prognosis v Nasal defects v Auricular defects v Orbital defects v Large midfacial defectsKey factor: During resection andclosure surgeon should attempt toleave adjacent tissues undisturbed
- 42. Alterations at Surgery to Enhance the Prosthetic Prognosis – Nasal DefectsThese are ideal defects. Why? v The nasal bones have been resected v The nasal labial folds are in normal position and of normal depth v Cheek contours are undisturbed v The upper lip is in normal position and of normal contour v The floor of the nose has been lined with skin v The anterior portion of the septum has been removed providing good access to the defect
- 43. Alterations at Surgery to Enhance the Prosthetic Prognosis – Nasal DefectsWith ideal defects such as these an excellentcosmetic result can be obtained and the prosthesiswill be well retained
- 44. Unfavorable nasal defects In this patient, primary closure of wound resulted in deficient lip contours and distortion of left nasolabial fold. The lip is retracted and elevated.
- 45. Unfavorable defect.Note deficient cheek lip contours and superior displacementof upper lip. Because of distortion of cheeks and retractionof lip, size and contours of prosthesis were made to becompatible with existing contours and did not reproducepreresection nasal size and contour. The angle formed lipand bottom of the nasal prosthesis is unfavorable
- 46. Unfavorable nasal defects The nasal bones have been retained and the lip was tied to the nasal mucosa resulting in significant superior retraction of the upper lip. It is not possible to fabricate an acceptable nasal prosthesis on such a patient.
- 47. Unfavorable nasal defects v Retention of the nasal bonesv Retraction of the upper lip Problems created a) Nasal bones affect position of the nasal tip b) Lip will always appear too short even if nasal tip of the prosthesis is shortened Result: Unesthetic c) Nasal prosthesis will always appear too prosthesis large because of the lip retraction and presence of the nasal bones
- 48. Unfavorable nasal defects Total rhinectomy defects better than partial rhinectomy defectsv Margins are more exposedv Distortions and displacement of residual nasal elements make it difficult to restore proper size and symmetry
- 49. Alterations at Surgery to Enhance the Prosthetic PrognosisLining the floor of the nose with a skin graft v Limits contracture and elevation of the upper lip v Maintains the position of nasolabial folds (the alar groove should blend continuously with nasolabial fold) v Provides a platform upon which the prosthesis sits
- 50. Alterations at surgery to enhance the prosthetic prognosisOrbital defects v Linethe orbit with skin v Avoid distortion of the eye brow v Do not close the defect with flaps v Do not retain the eyelids
- 51. Alterations at Surgery to Enhance the Prosthetic Prognosis Orbital DefectsThis orbital exenteration defect is close to ideal. Theentire contents of the orbit have been removed andthe orbital walls lined with skin. However, the positionof the eyebrow is somewhat distorted.
- 52. Alterations at Surgery to Enhance the Prosthetic Prognosis Orbital Defectsv Lateral facial orbital defect resurfaced with a free flap leaving sufficient space for an orbital prosthesis.v Orbital prosthesis in position.
- 53. Alterations at Surgery to Enhance theThe lids were retained following orbital exenteration. There isinsufficient space for an orbital prosthesis. If an orbitalprosthesis is contemplated, they should be removed.
- 54. Alterations at Surgery to Enhance the This orbital defect was filled with a flap. As a result, there is insufficient space for a prosthesis.
- 55. Alterations at Surgery to Enhance theThe eyebrow has been altered in this patientmaking it more difficult to restore facialsymmetry with an orbital prosthesis
- 56. Alterations at surgery to enhance the prosthetic prognosisEar defects v Total auriculectomy defects are easier to restore than partial auriculectomy defects v Retain the tragus v Line the defect with a split thickness skin graft v Avoid the use of flaps with hair follicles v When appropriate, place osseointegrated implants
- 57. Alterations at surgery to enhance the prosthetic prognosisv Retain the tragus.v Line site with split thickness skin graft. Why?The tragus helps hide the anterior margin of the prosthesis
- 58. a Alterations at surgery to enhance the prosthetic prognosis Unfavorable ear defects Large displaced ear fragments. Bilateral symmetry with opposite ear cannot be achieved with the prosthesis
- 59. Alterations at surgery to enhance the prosthetic prognosis Unfavorable ear defectsPartial ear defects are more difficult to restore because: v Blending margins is more difficult v Bilateral symmetry may be impossible to restore
- 60. Alterations at surgery to enhance the prosthetic prognosis Unfavorable ear defectsThis defect has been lined with a hair bearing scalp flap.Problems that result:v Difficult to use skin adhesivesv We are unable to place osseointegrated implants through skin with hair follicles.
- 61. Large Midfacial Defectsv Skin grafts should be used to line v All raw tissue surfaces v All potential support surfaces v All useful undercutsv Attempt to avoid distortion of facial contours adjacent to the defect. Avoid primary closurev If the upper lip is resected do not attempt to reconstruct itv Place implants at the time of surgical ablation
- 62. Large Midfacial DefectsSkin grafts should be used to line v All raw tissue surfaces v All potential support surfaces v All useful undercuts
- 63. Large Midfacial Defects Favorable vs Unfavorable Defect Skin lined vs nonskin lined defect a bCompare these two defects. In “a” the maxillary sinus is lined with respiratorymucosa and the septum has been retained. Such a defect cannot beeffectively engaged to help retain, support or stabilize the oral – facialprostheses. Patient “b” presents with a more favorable defect. The walls ofthe maxillary sinus have lined with skin and the septum has been removed.Hence, the defect can be positively engaged with the facial prosthesis tofacilitate retention, stability and support of the oral – facial prostheses.
- 64. Large Midfacial DefectsIf the more than half of the upper lip is resected do not attempt to reconstruct itProblemsvScarring of the reconstructed lip may limit oral accessvThe reconstructed upper lip retracts superiorly and is unable to interact effectively with the lower lip to achieve lip seal. Speech and saliva control are thereby rendered ineffectivevThe cosmetic result is usually unacceptable
- 65. Large Midfacial Defects a bIn the previous two patients the non functionalreconstructed lip was overlaid with the facialprosthesis. Both speech and the esthetic result wereenhanced. In patient (b) a moustache has been usedto camouflage the lip margin.
- 66. Large Midfacial Defects Placement of implants at the time of tumor resectionv Lateral portion of defect was restored with a free flapv Implants were placed at the time of tumor ablation. When the surgical site is healed the implants are fully osseointegrated and can be used to retain, stabilized and support the proposed oral – facial prostheses
- 67. Alterations at surgery to enhance the prosthetic prognosisAdvantages: Placement of implants at the time vLimits the number of surgeries of surgical ablation is particularly vAccelerates rehabilitation – When necessary when large facial the surgical site is healed and ready defects are anticipated for a prosthesis, the implants are osseointegrated
- 68. Alterations at surgery to enhance the prosthetic prognosisAdvantages: This practice is recommended vLimits the number of surgeries even if the patient is to receive vAccelerates rehabilitation – When postoperative radiation (see the surgical site is healed and ready lecture “Implants in Irradiated for a prosthesis, the implants are Patients”) osseointegrated
- 69. Basic Principlesv Form and symmetryv Surface texturev Lines of juncturev Coloration
- 70. Form and SymmetryIssues Ideal, and symmetrical contours? v Yes,but only if the defect is favorable. However, if there are significant distortions of existing facial contours, the prosthesis must be tailored accordingly Restore bilateral symmetry? v Usually not, particularly if the defect is unfavorable
- 71. Form and SymmetryIf the defect is favorable ideal symmetricalcontours are developed. Note the varioussizes, shapes, colors and surface textures
- 72. Form and Symmetry There were distortions of the existing facial contours in both of these patients and the prosthesis was adjusted to accommodate to these alterations.v Nasal defect with significant v Patient presented with naso- elevation of the lip on the right. labial fold higher on the right Nasal prosthesis in position. than on left. The note Right ala was reduced in size difference in size of ala and elevated to better blend with between right and left. existing contours.
- 73. Form and Symmetryv Maxillectomy-orbital exenteration defect. Note deficient cheek contours.v Orbital prosthesis in position. Symmetry is restored in orbital region but not in cheek. The contour of zygomatic-malar area was not restored. Cheek portion was blended with existing cheek contours.v Note how eyeglass frames and shadows cast by them help camouflage the defect.
- 74. Form and Symmetryv Contour of columellav The margin is visible on the upper lip. In most patients it is advisable to place margin beneath the height of contour of columella
- 75. Form and SymmetryAfter recontouring the columella and tucking itsmargin beneath the tip of nose the appearance of theprosthesis is improved.
- 76. Surface TextureA simple stipple is required for most ear prostheses.
- 77. Surface texture v Stipple, lines and grooves must be slightly more prominent than those on the adjacent skin. Why? v Some of the surface detail is lost during flasking, processing and the application of extrinsic colorants.
- 78. Surface Texture Orbital defects require much more surface detailLarge orbital defect. Surface texture of suborbital area andcheek have been faithfully reproduced. Note that texture ofsculpting is slightly more prominent than skin. This is so becausesome detail is lost during processing and extrinsic coloration.
- 79. Surface TextureProper surface texture for an orbital prosthesis.Note orbital skin folds are carefully reproduced.
- 80. Surface Texturev Ideal orbital exenteration defect. Defect is lined with skin, eyebrow is in reasonable position and adjacent facial contours are not distorted.v Orbital prosthesis in position. The globe is properly positioned, the lid contours are excellent as is the coloration.v What is lacking in this prosthesis? v Sub orbital skin texture has not been reproduced
- 81. Margins (Lines of Juncture)Nasal Defects v Blend alar groove with nasolabial folds v Hide columella margin beneath the nasal tip v Feather exposed margins v Hide exposed margins beneath eyeglass frames
- 82. Margins – Lines of JunctureNote the margins (lines of junction) are difficult to detect in these patients
- 83. Margins (Lines of Juncture) A BvTragus hides some of the anterior margin (A)vWithout a tragus the margin anteriorly is carefully thinned (B)vEar lobe margins represented by a line in the skin
- 84. Margins (Lines of Juncture) v The eye glass frames help to hide the margins of orbital prostheses v In this orbital prosthesis the surface texture has been faithfully reproduced
- 85. Coloration Intrinsic vs extrinsicI prefer extrinsic coloration to create and highlight thesurface detail because:vIt is easier to train residents in this technique as opposed to intrinsic coloration methodsvMore consistent esthetic results can be obtained with this methodvThis method is more time efficient. Multiple prostheses can be efficiently fabricated with this technique
- 86. Coloration – Extrinsic v Shade guides will ensure consistency in color and translucence of base. v Coloration is accomplished under corrected light conditions.
- 87. Coloration – Extrinsicv Small ear defect.v Prosthesis engages undercuts behind ear and in concha.v Completed prosthesis.
- 88. Coloration – Extrinsic Nasal and ear prosthesis. Note excellent color matching, surface texture reproduction and marginal adaptation.
- 89. Coloration – ExtrinsicShadows and skin creases must be embellished withpaint because of the translucence of the material.
- 90. Coloration – ExtrinsicShadows must be embellished with paintbecause of the translucence of the material
- 91. Coloration – Intrinsic a b cSome clinicians preferintrinsic methods dbecause:v The surface detail does not wear off as easily as compared to extrinsic methods.v Surface texture is better maintained
- 92. Coloration – Intrinsic a b c Method and Technique:v Catalyzed silicone colors (a). dv Painting initial color into mold (b).v Each layer is allowed to partially catalyze before the subsequent one is added (c)v Subsequent color layers in mold.v Base shade added to mold (d).
- 93. Coming soonvRestoration of nasal defectsvRestoration of auricular defectsvRestoration of orbital defectsvRestoration of midfacial defects
- 94. v Visit ffofr.org for hundreds of additional lectures on Complete Dentures, Implant Dentistry, Removable Partial Dentures, Esthetic Dentistry and Maxillofacial Prosthetics.v The lectures are free and available upon registering for the sitev Our objective is to create the best and most comprehensive online programs of instruction in Prosthodontics


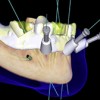 Computer Guided Treatment Planning and Surgery
Computer Guided Treatment Planning and Surgery
 Restoration of Posterior Quadrants and Treatment Planning
Restoration of Posterior Quadrants and Treatment Planning
 Implants and RPDs
Implants and RPDs
 Angled Implants
Angled Implants
