During the last 10 years the treatment of patients with radiation has changed dramatically. Biologically equivalent doses have been increased by 7-10 Gy by the use of concomitant chemoRT and postoperative doses have been increased dramatically. The methods used in radiation delivery have changed with the increased use of Intensity Modulated Radiation Therapy (IMRT). These changes have significantly increased post-radiation morbidity-(chemoRT), while some have decreased postradiation morbidity (IMRT). This program describes in detail these changes and how they impact dental care and maintenance.
Radiation of Head and Neck Tumors — Course Transcript
- 1. 1. Radiation of Head and Neck Tumors Robert Kagan, MD, Division of Radiation Oncology, Kaiser Permanente John Beumer III, DDS, MS Division of Advanced Prosthodontics,Biomaterials and Hospital Dentistry and the Jane and Jerry Weintraub Center for Reconstructive Biotechnology UCLA School of Dentistry All rights reserved. This program of instruction is covered by copyright ©. No part of this program of instruction may be reproduced, recorded, or transmitted, by any means, electronic, digital, photographic, mechanical, etc., or by any information storage or retrieval system, without prior permission of the authors.
- 2. Radiation of Head and Neck Tumorsv Introduction Table of Contentsv Biologic effectsv Modalitiesv Fractionationv Methods v CRT v IMRT v Brachytherapy v ChemoRTv Indications and key factsv Tissue changes v Immediate v Long term
- 3. Radiation of Head and Neck Tumors IntroductionChanges since the turn of the century v Doseescalation particularly with post-operative radiation therapy v Postoperative doses have increased from 50 Gy to 60 Gy and sometimes accompanied by concomitant chemotherapy v ChemoRT – Adds bio-equivalent of 7-10 Gy to the irradiated tissues and impacts the tissues out of the treatment volume as well. ” Post treatment morbidity dramatically increased!! ” Is immune surveillance compromised? ” Rate of development of second oral primaries and other cancers has not yet been studied? v IMRT ” Impact on salivary flow, the incidence of ORN,
- 4. Radiation of Head and Neck Tumors Impact of these changesv Preradiation dental screening v Dose and volume of tissues receiving the highest levels of dose will vary considerably from patient to patientv Acute side effects v The use of ChemoRT dramatically increases the acute side effects v The use of IMRT probably decreases the acute side effects
- 5. Radiation of Head and Neck Tumors Impact of these changesv Incidence of post treatment morbidity is rising ” Xerostomia – Probably not effected by IMRT because the relatively low doses (26-40 Gy) will severely damage the salivary gland parenchyma. ” Mucosal atrophy ” Caries ” Dysphagia and Trismus – Dramatically increased with the use of ChemoRT
- 6. Radiation of Head and Neck Tumors Impact of these changesv Incidence of post treatment morbidity is rising ” Trismus – Dramatically increased with the use of ChemoRT ” Velopharyngeal insufficiency and velopharyngeal incompetence – Dramatically increased with the use of ChemoRT ” Osteoradionecrosis – Dramatically increased with the use of ChemoRT when conventional radiation therapy is employed. Incidence still unknown when ChemoRT is used with IMRTv Current literature ” Is it particularly helpful given the changes? Not particularly.
- 7. Radiation of Head and Neck Tumors We also need to be familiar with the methods of radiation treatment used previously. v Conventional radiation v Hyperfractionation v Accelerated fractionation v BrachytherapyWhy? Because many postradiation patients present with dental issues andthe long term tissue effects are dependent on dose levels and the volume oftissues exposed high doses.
- 8. Biologic Effectsv Nucleus 100 to 1000 times more sensitive than the cytoplasmv Most damage ” Mitotic apparatus ” DNA
- 9. High Dose RadiationImmediate Cell Death Reproductive DNA Damage (Interphase Death (Functional Cell) Spontaneous Trauma Necrosis Induce Proliferation (Reproductive Death) Induced proliferation and cell death after irradiation.
- 10. Induced proliferation and cell death after irradiation. XRT
- 11. Modalitiesv External radiation therapy v Radiation is delivered via an external source v CRT – Conventional lateral facial fields that are usually equally weighted v IMRTv Brachytherapy v The modality of radiation therapy that utilizes radioactive isotopes within capsules, needles, tubing etc. inserted into body cavities (intracavitary) or into tissues and organs (interstitial).
- 12. External Radiation Therapy Photon beam therapy* v Superficial (50 keV to 150 keV) – was used for treatment of small superficial skin tumors v Orthovoltage (150 keV to 300 keV) – was used to treat superficial but thick tumors of the skin v Megavoltage (1 MeV or greater, like cobalt and linear accelerators) – used to treat deeply situated tumors while sparing superficial normal tissues (“skin sparing”)*Used for most oral and pharyngeal tumors
- 13. External Radiation Therapy Particulate Radiations v Electronbeam v Neutron beam v Proton beamElectron beam is the most commonly employed. It allowsfor delivery of high doses of radiation to tumors locatedwithin 6 cm of the surface. The energy of the beam canbe adjusted to the depth of interest. Neutron beam andProton beam therapy are not widely available and are stillconsidered experimental.
- 14. Mixed Beamv Combination of electron beam plus photon beamv Often used in the treatment of parotid tumors or large skin tumors
- 15. Units of Dosagev The unit of radiation dose is called the gray and is defined as the energy absorption of 1 joule per kilogram of tissue.v This has replaced the rad, which corresponds to to an energy absorption of 100 ergs/gm.v Therefore, 1 rad equals 1 centigray (cGy).
- 16. FractionationRadiation is delivered in a series of treatments orfractions. They average around 200 cGy per fractionand are generally delivered over a 6-7 week period.Total dose when conventional fractionation is used,ranges from 6600-7200 cGy.
- 17. Fractionation -Scientific rationale:v Allowsfor reoxygenation of hypoxic, radioresistant tumor cellsv Cell cycle dynamics v Redistribution of cells within the cell cycle tends to sensitize the more rapidly dividing cells in the tumorv Repopulation of cells between fractions permitting regrowth of normal cellsv Normal cell recovery vs tumor cell recovery v Normal cells have a greater capacity to repair sublethal damage than tumor cells
- 18. FractionationHyperfractionation v Number of fractions per day increases as does total dose, and the total number of fractions. Treatment time remains the same and dose per fraction averages about 120 cGy per fraction as opposed to 200 cGy used in conventional fractionated therapy.Accelerated fractionation v Slight decrease in the dose per fraction which ranges from 140 cGy to 160 cGy and is given twice or thrice daily. Overall dose is the same or less and treatment time is reduced.
- 19. Fractionation Schedules Dose Fractions Per Day TimeConventional 7000 35 200 times 1 7 weeksHyperfractionation 8050 70 115 times 2 7 weeksAccelerated 7200 45 160 times 3 3 weeksHyperfractionated/ 5400 36 150 times 3 12 days Accelerated
- 20. Fractionation HyperfractionationAcute side effects were more severe than conventionalfractionation protocols (Denham et al, 1999) but the late effectsappeared to be less although good clinical data is still notavailable. Hyperfractionation and accelerated fractionation were used primarily in the treatment of large unresectable tumors, such as this lesion, that ordinarily would be difficult to control with conventional fractionation protocols.
- 21. Changing methods of radiation deliveryConventional radiation therapy (CRT) l 200 cGy per fraction l Total doses l 7000 cGy definitive dose l 5000-6000 cGy post op Source: www.beaumonthospital.com Intensity modulated radiation therapy (IMRT) This technique uses multiple radiation beams of non-uniform intensities. The beams are modulated to the required intensity maps for delivering highly conformal doses of radiation to the treatment targets, while limiting dose to adjacent tissues.Source: www.beaumonthospital.com
- 22. DosimetryThe purpose of dosimetry is to evaluatethe amount of energy absorbed by thetissues subjected to radiation Isodose curvesv Graphic displays of dose patterns through tissuesv These characteristics will vary with the type and the energy of the radiation applied and can vary significantly between machines used to generate these beams
- 23. Isodose CurvesHigh energy photons are used primarily for deeply situated tumors whereasparticulate beam is used for more superficial tumors. Sometimes they areused in combination. Photon Beam Cobalt 60 Particulate Radiation – Electron Beam Isodose of photon beam Isodose curves of electron beam. Note rapid (Co60). Note progressive falloff of tissue dose. falling off of tissue dose and that maximum dosage level (100%) is attained below skin High energy photons are skin sparing surface
- 24. Isodose Curves Multiple Beamsv Prior to IMRT multiple beams were used to treat deeply situated tumors in order to deliver a dose to the tumor equal to or higher than the dose delivered to adjacent normal tissuesv Concentration of dose was achieved by using two converging photon beams and wedges (tumor of ethmoid and maxillary antrum).
- 25. Methodsv CRT v Radiation is delivered via bilateral opposed equally Source: www.beaumonthospital.com weighted fieldsv IMRT v Radiation delivered externally from multiple angles Source: www.beaumonthospital.comv Brachytherapy v Radioactive sources are implanted locally within the tissues encompassed by the tumor
- 26. Conventional Radiation (CRT) External Radiation – Fields Size, extent and clinical ramifications Simulation film Port filmPrior to the advent and widespread use of IMRT, most oral cavity tumors weretreated with bilateral opposed, equally weighted fields. This field was used totreat a patient with a nasopharyngeal carcinoma. Note how the field has been reshaped to avoid the mandibular molar area.
- 27. Conventional Radiation (CRT) External Radiation – Fields Size, extent and clinical ramifications Simulation film Port filmThe high posterior fields used for treatment of soft palate, tonsillar andnasopharyngeal tumors include substantial portions of the parotid glands andsubmaxillary glands. The resultant reduction in salivary flow predisposes toradiation caries. The risk of osteoradionecrosis, however is low when this typeof field was used.
- 28. Conventional Radiation (CRT) External Radiation – Fields Size, extent, and clinical ramifications Simulation film Port filmOpposed mandibular fields seen here were used to treat tumors arisingfrom the floor of the mouth and anterior two thirds of the tongue. Theyexpose most of the mandibular body to high doses of radiation and as aresult the risk of osteoradionecrosis is high. However, in these patientsmuch of the parotid glands are spared. Consequently, the risk of cariesis reduced.
- 29. Conventional Radiation (CRT) External Radiation – Fields Simulation Initial Radiation Off Cord Boost Film Field Field FieldDuring treatment radiation fields were often reduced in size. Forexample, the initial field is used to carry the dose to 5000 cGy. The“off cord” field brings the tumor dose to 5500 – 6000 cGy. The boostfield encompasses only the primary lesion and brings the tumor doseto approximately 7000cGy.
- 30. Intensity modulated radiation therapy (IMRT)Advantages: Reducing the dose local tissuesreceive from high dose radiation such as salivaryglands and boneConcerns: Underdosing the primary tumor andnodal areas
- 31. IMRTv IMRT dose distribution diagrams. Note that higher dose per fractions are centered on clinical tumor volume. Note how parotid tissues receive a lower dose.v If parotid dose (pink) can be kept below 30 Gy postradiation salivary flow will be close to normal.
- 32. IMRTSource:www.Beaumonthospitals.com
- 33. IMRT dosimetry diagramsNote the hot spot on anterior mandible (oval)
- 34. BrachytherapyDefinition – The modality of radiation therapythat utilizes radioactive isotopes within capsules,needles, tubing etc. inserted into body cavities(intracavitary) or into tissues and organs(interstitial).
- 35. Brachytherapyv Iridium 192 seeds are most commonly used today. They are used primarily in T1 and T2 localized carcinomas of the oral tongue and floor of the mouth.v Most patients receive 5000-5500 cGy of external beam to the tumor volume and the nodal bed followed by a boost provided with brachytherapy.Advantages: v Dose to the buccal side of the mandible on the side of the tumor is generally limited to the dose delivered by the external therapy. This level (5000-5500cGy) of radiation is not sufficient to totally eliminate the fine vasculature of these tissues.
- 36. Isodose Curves – BrachytherapyIsodose curves of iridium implants positioned in the floor ofthe mouth. Note rapid falloff of tissue dose as distance fromsources increase. As a result the tissue effects of theradiation are localized. The oral mucositis is confined to thetissues in and around the implant.
- 37. Brachytherapy – Clinical SignificancePrior to therapy teeth on the side opposite the implant can be treatedmore conservatively than those adjacent to the implant. Teeth adjacentto the implant should be considered for removal prior to therapy.
- 38. Chemoradiation (CRT) (IMRT) Source: www.beaumonthospital.com Source: www.beaumonthospital.com v In combination with CRT or IMRT v Full course of concomitant chemoradiation is theoretically equivalent to an additional 700-1000 cGy (Kashibhatla, 2007, Fowler, 2008).Consequences (particlularly with CRT): More short term and long term side effects (mucositis, trismus, dysphagia,velopharyngeal function, osteoradionecrosis).
- 39. Indications and key facts Most malignant neoplasms of the mucosa of the head and neck arev squamous carcinomas of various radio- sensitivities.v Primary lymphomas and adenocarcinomas are relatively rare.v Sarcomasand melanomas are also rare and are primarily surgicaldiseases that require wide margins. These margins may not be possible inthe head and neck region without undue morbidity, so treatment oftencombines surgery and postoperative radiotherapy.
- 40. Indications and key factsv Chemoradiation is generally the treatment of choice for carcinomas arising from the nasopharynx, base of tongue, tonsil and soft palate because of surgical morbidity or difficult access.v Carcinomas of the alveolar ridge and salivary glands should be treated surgically, due to the potential for bone I infiltration (alveolar ridge), and then possibly followed by radiation therapy.
- 41. Indications and key factsv Early carcinomas of the tongue and floor of mouth are equally wellcontrolled with either surgery or radiation therapy.v When conventional fractionation and external radiation is useddoses are in the order of 6600 to 7200 cGy in 6 to 7 weeks.v Local tumor doses from interstitial therapy can be higher.
- 42. Indications and key factsv Lymphnode metastases are fairly radiocurable when they are less than 2 cm in diameter.v Tumorsexhibiting deep invasion of soft tissue or extension into bone or cartilage are less likely to be controlled with radiation alone, and a planned combined approach with surgery and/or chemotherapy may be considered.
- 43. Indications and key factsIndications for postoperative radiotherapyinclude: v Positive and/or close surgical margins v Residual gross disease v Tumor spillage v Perineural invasion v Lymphovascular invasion v Multiple positive nodes v Extracapsular extension v The known recurrence pattern
- 44. Immediate Tissue ChangesSeconds, minutes, hours after initial exposure v Free radical formation v Disruption of molecular bonds v Breaks in DNA strands
- 45. Initial Tissue Effects – Early Changesv Swelling, degeneration and necrosis of the inner endothelial lining of small arteries and arterioles.v Loss of endothelial lining leads to formation of thrombi which occlude the smaller vessels.v These changes lead to increased permeability of vessel walls which in turn leads to increased vascular congestion.v Increased amounts of perivascular fluid exerts pressure on the walls of small vessels further impeding blood flow. Result: Metabolic support for surrounding tissues is impaired leading to fibroblastic activity and fibrosis.
- 46. Long Term Tissue Changesv Cardiovascular system – Blood vesselsv Musculoskeletal systemv Hematopoietic tissuev Skin and mucosa
- 47. Long Term Tissue ChangesBlood Vessels*# v Microcirculation v Thrombosis Results in net v Telangiectasia loss of vascular networks v Occlusion of vessel lumens v Small and medium sized arteries v Formation of intimal fibrotic plaques Results in v Fibrosis of the muscular walls anoxia, cell v Foam cell plaques in the intima death and v Perivascular fibrosis fibrosis*These changes, are responsible for many of the injurious sideeffects of radiation on a variety of cells and body tissues.#The cells most responsible for the long term damage arefibroblasts and the intimal cells of the blood vessels.
- 48. Late Effects – TelangiectasiaTelangiectasiav Represents dilation and coalescence of capillaries and small venules in the lamina propria (mini aneurysms). They have been described as a contraction of 10-20 capillaries into one microaneurysm. Telangiectasias significantly reduce blood flow to the area.v Indicates that the epithelium is 5-6 cell layers thick and is easily perforated
- 49. Long Term Tissue ChangesMusculoskeletal system v Bone ” Trabeculae loose their osteocytes ” Marrow becomes avascular, acellular and fibrotic ” Continued osteoclastic activity ” Periosteum exhibits fibrosis with atypical fibroblasts
- 50. Long Term Tissue ChangesMusculoskeletal system Muscle v Atrophy – v Velopharyngeal incompetence v Impaired tongue function v Fibrosis and Muscle contracture v Trismus v Pain with motion
- 51. Long Term Tissue Changesa bExamples of muscle wasting and fibrosis of heavily irradiated tissues. a: Patient presented with velopharyngeal insufficiency with hypernasal speech and nasal leakage during swallowing. b: Patient presented with compromised speech articulation secondary to reduced bulk and mobility of tongue.
- 52. Long Term Tissue ChangesHematopoietic tissue Very radiosensitive v Fatty and fibrous degeneration v Complete absence of hemopoietic activity v Loss of stem cells v Negative impact on osseointegration
- 53. Long Term Tissue ChangesSkin v Atrophy v Hyperpigmentation or depigmentation v Dryness v Alopecia v Chronic ulceration v Scarring v Telangiectasia
- 54. Long Term Tissue Changesv Velopharyngeal insufficiency – Secondary to muscle wasting and fibrosisv Cranial neuropathies – Secondary to fibrosis of the nerve trunk and loss of myelin sheathsv Caries – Secondary to compromise of the quality and quantity of saliva. Loss of salivary parenchyma is primarily caused by fibrosis and loss of its vasculature.v Trismus – Secondary to contracture of the muscles of mastication secondary to fibrosis and atrophy associated with the loss of vasculature.
- 55. v Visitffofr.org for hundreds of additional lectures on Complete Dentures, Implant Dentistry, Removable Partial Dentures, Esthetic Dentistry and Maxillofacial Prosthetics.v The lectures are free.v Our objective is to create the best and most comprehensive online programs of instruction in Prosthodontics
- 56. Referencesl Kasibhatla M, Kirkpatrick J, Brizel D. (2007) How much radiation is the chemotherapy worth in advanced head and neck cancer. Int J Radiat Oncol Biol Phys 68:1491-95.l Fowler J, Stern B. (1963) Dose time relationships in radiotherapy and the validity of cell survival curve models. Br J Radiol 36: 163-173.l Fowler JF. (2008) Correction to Kasibhatla et al. How much radiation is the chemotherapy worth in advanced head and neck cancer. Int J Radiat Oncol Phys 71:326-9.l Elkind M, Sutton H. (1959) X-ray damage and recovery in mammalian cells in culture. Nature 184:1293-5.l Kaliman R. (1972) The phenomenon of reoxygenation and its implication for fractionated radiotherapy. Radiology 105:135-42.l Ellis, R. (1968) Relationship of biologic effect to dose-time: fractionation factors in radiotherapy. Current topics in radiation research, Vol. 4. Amsterdam, North Holland Publishing Co. pp. 357-97.l Hall E. (2006) Radiobiology for the radiobiologist. ed 6 Philadelphia: Lippincott, Williams and Wilkins.
- 57. Referencesl Powers B, Gillette E, McChesney S, et al. (1991) Muscle injury following experimental intraoperative irradiation. Int J Radiat Oncol Biol Phys 20:463-71.l Eisbruch A, Lyden T, Bradforn C, et al. (2002) Objective assessment of swallowing dysfunction and aspiration after radiation concurrent with chemotherapy for head and neck cancer. Int J Radiat Oncol Biol Phys 53:23-8.l Nguyen NP, Frank C, Moltz CC, et al. (2006) Aspiration rate following chemoradiation for head and neck cancer: an underreported occurrence. Radiol Oncol. 80:302-6.l Nguyen NP, Frank C, Moltz CC, Vos P, Millard C, et al. (2008) Dysphagia severity and aspiration following postoperative radiation for locally advanced oropharyngeal cancer. Anticancer Res 28:431-4.l Nguyen NP. Analysis of factors influencing aspiration risk following chemoradiation for oropharyngeal cancer. Brit J Radiol 82:675-80l Kinsella T, Deluca A, Pezeshkpour G, et al. (1991) Threshold dose for peripheral nerve following intraoperative radiotherapy (IORT) in a large animal model. Int J Radiat Oncol Biol Phys 20:697-701.
- 58. Referencesl Fajardo L-G, L Bertrong M, Anderson R. (2001) Nervous system. In Radiation Pathology. Eds Fajardo L-G, L Bertrong M, Anderson R Oxford University Press pp 362-3.l Scrimger JW. (1977) Back scatter from high atomic number materials in high energy photon beams. Radiology 124:815-17.


 Prosthodontic Procedures and Complications
Prosthodontic Procedures and Complications
 Angled Implants
Angled Implants
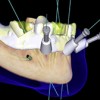 Computer Guided Treatment Planning and Surgery
Computer Guided Treatment Planning and Surgery
 Restoration of Posterior Quadrants and Treatment Planning
Restoration of Posterior Quadrants and Treatment Planning
