Given their demographic profiles most patients with oral cancer present with significant dental disease prior to radiation therapy. If left unattended diseased dentition may cause serious dental infections after therapy. As a result, pre-radiation dental evaluation has become an integral part of care offered to those patient about to receive cancericidal doses of radiation for head and neck tumors. This program discusses the role of preradiation extraction and the criteria used to determine which teeth, if any, require removal prior to initiation of radiation treatment.
Maxillofacial Prosthetics – Preradiation Dental Assessment — Course Transcript
- 1. 5. Preradiation Dental Assessment Criteria for Extractions John Beumer III, DDS, MS Eric Sung, DDS Division of Advanced Prosthodontics,Biomaterials and Hospital Dentistry and UCLA School of DentistryAll rights reserved. This program of instruction is covered by copyright ©. Nopart of this program of instruction may be reproduced, recorded, or transmitted,by any means, electronic, digital, photographic, mechanical, etc., or by anyinformation storage or retrieval system, without prior permission of the authors.
- 2. Preradiation extractionsv Given their demographic profiles most patients with oral cancer present with significant dental disease prior to therapyv If left unattended diseased dentition may precipitate serious infections after therapyv The primary purpose of preradiation dental extraction is to minimize the risk of dental infection leading to an osteoradionecrosis after therapy.
- 3. Preradiation extractionsv Key issue is still dose and volumev Up until a few years ago dose and volume were easy to determine prior to therapyv Today, this has become quite difficult. Why? v IMRT v Chemoradiation
- 4. Preradiation Dental ConsultationPurpose: a) Inform the patient that because of tissue changes and reduction of salivary flow that he/she will be more susceptible to dental caries and dental and bony infection after radiation therapy. b) Examine the dentition and determine which teeth are salvageable and which teeth need to be removed. c) Explain to the patient the importance and the methods used for optimal dental compliance.
- 5. Preradiation Dental EvaluationWhat is the role of preradiation extractionin the prevention of osteoradionecrosis?
- 6. Preradiation Extractions The UCLA Philosophyv Most authors believe selected tooth removal prior to radiation therapy, particularly mandibular molars in the field demonstrating furcation involvement, will reduce the rate of osteoradionecrosis (ORN) and minimize the risk of a patient developing a discontinuity defect secondary to ORN (Silverman and Chierici, 1965; Hayward, 1969; Beumer et al; Epstein et al, 1997; Bruins et al, 1999; Vissink et al, 2003). Why?
- 7. Preradiation Extractions The UCLA Philosophyv Wholesale extraction of healthy teeth in the field, particularly in a compliant patient, is not recommended and probably increases the rate of osteoradionecrosis (ORN).v ORN that develops in association with residual mandibular dentition is difficult to control with conservative therapy and often leads to resection of large mandibular segments.v ORN secondary to postradiation extractions likewise is difficult to control with conservative therapy and often leads to resection of large mandibular segments.
- 8. Preradiaton Extractions – Rationalev The rate of ORN secondary to preradiation extractions is less than 10%.v ORN caused by preradiation extractions are almost always treated successfully with conservative means with retention of mandibular continuity whereas ORN secondary to postradiation extraction or infections associated with teeth frequently lead to loss of major segments of the mandible.
- 9. Preradiaton Extractions – Rationalev Therefore, it is logical to assume that extraction of diseased mandibular teeth within the radiation field will not only reduce the rate of ORN but also minimize the morbidity of ORN secondary to its treatment.
- 10. Preradiaton Extractions – Rationalev For example, this patient presented with an ORN several months following radiation at the site of a preradiation extraction. This exposure was of 4 months duration. The nonvital bone eventually sequestrated and the site covered with normal epithelium after 8 months of conservative therapy.
- 11. Preradiation Extraction – Rationalev The ORN rate in dentulous patients associated with mandibular teeth left in the field exceeds 25% (Murray et al, 1980).v Most of these ORN’s are precipitated by dental disease post radiation.v The rate of ORN secondary to postradiation extraction exceeds 30% in most studies (Beumer et al, 1984; Marx et al, 1985).v A substantial number of the ORN’s caused by dental disease and postradiation extraction result in resection of the affected portion of the mandible resulting in a discontinuity defect.
- 12. Preradiation Extraction – Rationalev In “A” the ORN developed as a A result of a periodontal abscess. In “B” the ORN was precipitated by post radiation extractions. These patients received 6800 cGy and 7000cGy respectively. Both patients eventually lost their mandibles on the affected side. Bv The course and progression of these two ORN’s is typical of those associated with postradiation extraction or acute periodontal infections, even if hyperbaric oxygen treatment is used.
- 13. Criteria for Preradiation Extractions Supporting Data
- 14. Preradiation extractions Number of patients 120 Osteoradionecrosis directly associated with extraction sites 12Only one of the 12 patients developing ORN associatedwith preradiation extractions required mandibular resectionand developed a discontinuity defect of the mandible. From Beumer et al, 1984
- 15. *From Beumer et al, 1983 Postradiation extractions – External beam dose and mandibular exposures*Dose Extraction Bone exposures Bone exposures Radical(cGy) episodes in excess of healed with resection of (mandible) 3 mths (mandible) conservative measures mandible0-4999 3 0 (0%) – -5000-5499 4 1 (25%) 1 -5500-5999 6 2 (33%) 2 -6000-6499 10 2 (20%) 2 -6500-6999 13 4 (31%) – 47000- 4 2 (50%) 1 1Totals 40 11(28%) 6 5 Note the high rate of mandibular resection
- 16. Postradiation Extractions No. (%) of No. (%) of ptsGroup No. Pts No. teeth sockets with ORN with ORNPenicillin 37 135 31 (22.9) 11 (29.9)Hyperbaric 37 136 4 (2.6) 2 (5.4)oxygen*Incidence of ORN following tooth removal in irradiatedpatients (Tumor doses were 6800 cGy or greater).*From Marx R, Johnson R and Kline S, 1985
- 17. Postradiation extractions* *In these clinical reports the dose to bone was in excess of 6500 cGy and the patients did not receive HBO.Incidence of osteoradionecrosis secondary to postradiation extractions Patients Osteos Grant and Fletcher, 1966 16 7 44% Beumer et al, 1984 40 11 28% Morrish et al, 1980 18 11 61% Marx, et al, 1984 37 11 30% Totals 111 40 36%
- 18. Criteria for Preradiation Extractions Based upon: v Dental disease factors v Radiation delivery factors
- 19. Criteria for Preradiation ExtractionsDental disease factors • Condition of the residual dentition • Advanced caries • Periapical infection An aggressive policy of • Periodontal bone loss extraction is recommended in these situations • Furcation involvement • Dental compliance of the patient • An aggressive policy of extraction is recommended in patients with poor dental compliance • Maxillary teeth vs mandibular teeth • Mandibular teeth are scrutinized more closely than maxillary teeth since maxillary teeth in the field can be extracted post radiation with minimal risk of osteoradionecrosis
- 20. Criteria for Preradiation Extractions Radiation Delivery Factors v Urgency of treatment v Mode of therapy v Clinical target volume (radiation) v BED (biologic equivalent dose) v Prognosis
- 21. Criteria for preradiation extraction (cont’d)Condition of the residual dentition v Furcationinvolvement (red arrows)of mandibular molars within the gross tumor volume if the dose is above 5500 cGyIn times past, periodontal abscesses were a primeinitiator of osteoradionecrosis, and the osteos (arrows)initiated in this manner frequently led to resection ofmajor portions of the mandibular body.
- 22. Criteria for preradiation extraction (cont’d)Condition of the residual dentition v Furcation involvement of mandibular molars within the gross tumor volume if the dose is above 5500 cGy In times past, periodontal abscesses were a prime initiator of osteoradionecrosis, and the osteos (arrows) initiated in this manner frequently led to resection of major portions of the mandibular body.
- 23. a bl Periodontal infection led to osteoradionecrosis in this patient.
- 24. Criteria for preradiaton extraction (cont’d)Periapical infections and advanced cariesAll teeth with suchadvanced pathologyshould be extracted.
- 25. Criteria for preradiation extractions (cont’d) History of poor dental complianceGiven the nature of the oral cancer population it is not surprising that substantialnumbers of patients will be noncompliant (Sennhenn-Kirchner et al, 2008) and so theless motivated the patient, the more aggressive one should be in the extraction ofmandibular teeth exposed to high dose (above 55 Gy) prior to therapy.If the patient has a history of poor dental compliance or if the clinicianquestions the patient’s ability or commitment to carry out the necessary oralhygiene maneuvers, an aggressive approach to preradiation extraction isrecommended. In this patient full mouth extractions were performed prior totherapy.
- 26. Criteria for preradiation extractions (cont’d) History of poor dental complianceNote the plaque accumulations, the periodontal bone loss and the class Vrestorations in these two patients. All these are signs of poor oral compliance. A BBoth these patients presented with squamous carcinomas of theright lateral tongue and both were scheduled to be treated withexternal beam therapy.In patient “A” all the remaining teeth wereremoved prior to therapy. In patient “B” the mandibular molarswere removed.
- 27. Criteria for preradiaton extractions (cont’d)ComplianceIf patients lack the dexterity or the will to usehygiene aids, at the very least, mandibular teethwithin the radiation field should be removed
- 28. Criteria for preradiation extractions (cont’d)Mandibular teeth vs Maxillary teeth Key factors to consider v The maxilla has a better blood supply than the mandible. v Maxillary teeth can be removed postradiation from the maxilla with little risk of the patient developing an ORN. Even if the patient does develops ORN they heal spontaneously causing little morbidity or deformity. v Removal of mandibular teeth in the field following radiation, if the dose to bone is above 6500 cGy, is extremely hazardous. The rate of ORN is 30-40% and many of these require resection of the involved portion of the mandible.
- 29. Criteria for preradiation extractions (cont’d)Mandibular teeth vs Maxillary teeth Therefore, we think that mandibular dentition should be scrutinized more carefully than the maxillary dentition prior to radiation for pretreatment extractions. Extraction of maxillary teeth with marginal pathology can often be deferred until after radiation therapy
- 30. Criteria for preradiation extractions (cont’d) Urgency of treatmentSome patients present with large anaplastic, rapidly growingtumors that need immediate treatment. In such patients dentalextractions need to be deferred.* Control of the tumor is obviouslythe most important consideration.*This situation occurs very rarely. When it does both theradiation therapist and the dentist must accept the risk offuture dental complications.
- 31. Criteria for preradiation extractions (cont’d) Mode of Therapy CRT vs IMRT vs Combined external beam and brachytherapy v Factors to consider v When brachytherapy is used all patients receive 5000-5500cGy of external beam therapy. v Below 5500 cGy vascular damage to the mandible is not profound, i.e. teeth can be removed from the field with little risk of osteoradionecrosis in most patients. v Brachytherapy boosts the dose delivered to the primary site by 2500-3500 cGy. v This boost is confined to the local tumor volume and so, much of the adjacent normal tissues are spared. v Risk of osteoradionecrosis in the mandible adjacent to the implant is very great.Clinical significance for patients with combinedexternal beam and brachytherapy: a) Teeth opposite the implant site can be viewed from a more conservative perspective b) Teeth adjacent to the implant need to be removed prior to radiation therapy
- 32. Criteria for preradiation extractions (cont’d) Mode of Therapy CRT IMRTv IMRT focuses radiation to gross tumor volume resulting in adjacent tissues receiving lower dose. Note how radiation is more focused around tumor when compared to CRT.
- 33. Criteria for preradiation extractions (cont’d)CRT – Radiation fields The more of the body of the mandible in the field the greater the risk of osteoradionecrosis and therefore the more aggressive one should be in removing teeth prior to therapy Planning film Port film Opposed mandibular fieldsMandibular molars should be very carefully scrutinized in such patients and if theydisplay evidence of periodontal pathology, they should be considered for removal.The risk of caries is low, particularly if a radiation stent is used to depress the tongueduring the therapy. These devices permit lowering of the radiation field thereby sparingparotid tissue and the palatal glands. Increased salivary flow decreases the caries rate.
- 34. Criteria for preradiation extractions (cont’d CRT – Radiation Fieldsv Patients with carcinomas of the lateral tongue and floor of the mouth are treated with opposed mandibular fields. These fields can be lowered with a tongue depressor-bite opener , sparing some parotid tissue, but the entire body of the mandible will still be in the radiation field. In these patients the dentition must be scrutinized very carefully and if the mandibular molars demonstrate significant periodontal deficiencies, they should be removed prior to therapy.
- 35. Criteria for preradiation extractions (cont’d) CRT – Radiation fields High posterior lateral facial fieldsPlanning Port High posterior fields such as thesefilm film include most of all the major and much of the minor salivary gland parenchyma. Salivary flow rates are reduced as much as 95% in patients treated with such fields and therefore the risk of caries is very high. The rate of osteoradionecrosis is low, because very little of the body of the mandible is in the field of radiation. Therefore, a more conservative approach to preradiation extractions can be used.
- 36. Criteria for preradiation extractions (cont’d) Mode of Therapy CRT IMRTv Since the high dose areas are confined to the clinical target volume, the dose to the opposite side is reduced.v The reduced volume of tissue exposed to high dose appears to reduce the risk of osteoradionecrosis (Studer et al, 2006; Ben- David et al, 2007).
- 37. Criteria for preradiation extractions (cont’d) Mode of TherapyIMRT v Therefore, one can be more conservative with regard to extraction of teeth on the side opposite the tumor. v However, the clinician must still be aggressive with regards to scrutiny of the dentition on the tumor side, particularly in the mandible.
- 38. a bv IMRT dose distribution diagrams. Note that higher dose per fractions are centered on clinical tumor volume.v Note how parotid tissues receive a lower dose. If parotid dose can be kept below 30 Gy postradiation salivary flow will be close to normal. In this case, dose was reduced to less than 50% of the tumor dose.v Extractions are dependent on the gross tumor volume and the dose delivered to this volume
- 39. Criteria for preradiation extractions (cont’d) IMRT – Gross Tumor Volume (GTV)v Highest levels of dose delivered to gross tumor volume (GTV)v Volume of mandible exposed to high levels of dose (above 6500 cGy) will determine the risk of ORNv The volume of the major salivary glands exposed to doses in excess of 4000cGy determines the degree of xerostomia anfthe risk of caries
- 40. Criteria for preradiation extractions (cont’d) Prognosis for tumor control If the intent of therapy is palliation, efforts should be directed towards pain control and maintenance of existing dentition. Extractions are only recommended for pain relief.This patient has a large lymph node that is fixed to underlyingstructures. The node and the primary tumor are unresectable and thetumor mass too large to be controlled with radiation therapy.Extractions are only indicated for pain control. Dentition should beretained to maximize function during his remaining days.
- 41. Criteria for preradiation extractions (cont’d)Dose to bone v When dose to bone to the mandible gets above 6500 cGy using conventional fractionation, the risk of ORN increases dramatically. Chemotherapy further increases the biologically equivalent dose (BED) by 700 to 1000 cGy (Kasibhatla et al, 2007; Fowler, 2008). v Asthe dose increases the clinician should be more aggressive in removing mandibular teeth within the field prior to therapy
- 42. Dose to BoneIncidence of bone necrosis according to dose* Incidence of bone necrosisDose to bone Dentulous patients Edentulous patients<6500 0/36 (0%) 0/3 (0%)6500-7500 8/29 (28%) 1/15 (7%)>7500 11/13 (85%) 2/4 (50%)Total 19/78 (24%) 3/22 (14%)* Morrish R, et al. Cancer 47:1980-8,1981
- 43. Preradiation ExtractionsSurgical procedures v Radical alveolectomy v Edges of the mucoperiosteal flaps should be freshened, the edges everted and primary closure obtained* v Teeth should be removed in segments to facilitate primary closure v Antibiotic coverage v Seven to ten days of healing required prior to radiotherapy*The lingual flap in the mandible is susceptible to mishandlingduring the procedure and perforation or thinning may lead to abony exposure during or after therapy.
- 44. Preradiation extractions (cont’d)Radical alveolectomy and primary closure Rationale v Mucosalhealing is occurs more rapidly v Remodeling apparatus after radiation is compromisedA radical alveolectomy was notperformed on this patient. Note theirregular bony bearing surfaces. Thesesharp bony projections will not remodelafter therapy and therefore this patientis not a candidate for completedentures.
- 45. Preradiation extractions (cont’d)Healing time is based on:v Nature of the infection associated with the dentition and the surrrounding bone – more infection requires more healing time.v Size of the surgical wound – larger wounds require more healing time.v Trauma inflicted during extractions, i.e. amount of bone removed during the alveolectomy. More surgical trauma requires more healing time.v Individual patient factors. Smokers may require extended healing periods.
- 46. Preradiation extractions (cont’d) Extraction of Third Molarsv Bony impactions – Extraction of impacted third molars is not advocated for most patients. Such extractions create large bony defects which may take several weeks to heal and may delay radiation therapy.v In this patient there appears to be a layer of bone over the top of the third molar.
- 47. Preradiation extractions (cont’d) Extraction of Third Molarsv Bony impactions` As noted previously extraction of impacted third molars is not advocated for most patients. However in this patient extraction of the 1st and 2nd molars exposed the third molars to the oral cavity and so they were removed.
- 48. Preradiation extractions (cont’d) Extraction of Third Molars Bony impactions – Note the third molar (arrow). Following removal, a radical alveolectomy was performed and the wound closed primarily.Extra time was required for this wound to heal prior to radiationtherapy- in this patient three weeks were necessary beforetreatment commenced.
- 49. Preradiation extractions (cont’d)Extraction of Third Molars v Partially impacted third molars represent a particularly perplexing problem. What would you recommend for this patient? Root canal therapy was performed on the second molar, thereby avoiding extraction of the third molar. The crown was amputated to facilitate oral hygiene.
- 50. v Visitffofr.org for hundreds of additional lectures on Complete Dentures, Implant Dentistry, Removable Partial Dentures, Esthetic Dentistry and Maxillofacial Prosthetics.v The lectures are free.v Our objective is to create the best and most comprehensive online programs of instruction in Prosthodontics
- 51. Referencesl Studer G, Furrer K, Davis BJ (2006) Postoperative IMRT in head and neck cancer. Radiat Oncol 1:40l Ben-David M, Diamante M, Radawski J. et al. (2007) Lack of osteoradionecrosis of the mandible after intensity modulated radiotherapy for head and neck cancer: Likely contributions of both dental care and improved dose distribution. Int J Radiation Onc Biol Phys 68:396-402.l Hayward J. (1969) The management of teeth related to treatment of oral cancer. CA- A Cancer Journal for Clinicians. 19:98-106.l Epstein J, van der Meit E, McKenzie M, et al. (1997) Postradiation osteonecrosis of the mandible. Oral Surg Oral Med Oral Path Oral Radiol Endod 83:657-62.l Bruins H, Jolly D, Koole R. (1999) Preradiation extraction decisions in patients with head and neck cancer. Oral Surg Oral Med Oral Path Oral Radiol Endod 88:406-12.l Beumer J, Silverman S, Benak S. (1972) Hard and soft tissue necroses following radiation therapy for oral cancer. J Prosthet Dent 27:640-44.l Daly T, Drane J. (1972) Management of dental problems in irradiated patients. Houston, Texas (Publication of the University of Texas).l Murray C, Herson J, Daly T, et al. (1980a) Radiation necrosis of the mandible: A 10 year study. Part I. Factors influencing the onset of necrosis. J Radiat Oncol Biol Phys 6:543-8.
- 52. Referencesl Murray C, Herson J, Daly T, et al. (1980b) Radiation necrosis of the mandible: A 10 year study. Part II. Dental factors: onset, duration and management of necrosis. J Radiat Oncol Biol Phys 6:549-53.l Mendenhall W. (2004) Mandibular osteoradionecrosis. J Clin Onc 22:4867-68.l Oh H, Chambers M, Martin J et al. (2009) Osteoradionecrosis of the mandible: Treatment outcomes and factors influencing the progress of osteoradionecrosis. J Oral Maxillofac Surg 67:1378-86.l Sennhenn-Kirchner S, Freund F, Grundmann S et al. (2009) Dental theapy before and after radiotherapy: An evaluation of patients with head neck malignancies. Clin Oral Invest 13:157-64.l Studer G, Studer S, Zwahlen R, et al. (2006) Osteoradionecrosis of the mandible: Minimized risk profile following intensity modulated radiation therapy (IMRT). Strahlenther Onkol 182:283-88.l Glanzmann C, Gratz K. (1995) Radionecrosis of the mandible: A retrospective analysis of the incidence and risk factors. Radiother Onc 36:94-100.l Annane D, Depondt J, Aubert P et al. (2004) Hyperbaric oxygen therapy for radionecrosis of the jaw: A randomized, placebo-controlled, double blind trial from the ORN96 group. J Clin Oncol 22:4893-4900.l Beumer J, Harrison R, Sanders B, et al. (1983b) Postradiation dental extractions: A review of the literature and a report of 72 episodes. Head and Neck Surg 6:581-6.
- 53. Referencesl Morrish R, Chan E, Silverman S, et al. (1981) Osteoradionecrosis in patients irradiated for head and neck cancer. Cancer 47:1980-3.l Thorn J, Hansen H, Specht L, et al. (2000) Osteoradioncecrosis of the jaws: Clinical characteristics and relation to the field of radiation. J Oral Maxillofac Surg 58:1088-93.l Del Regato, BOA. (1939) Dental lesions observed after roentgen therapy in cancer of the buccal cavity, pharynx, and larynx. Am J Roentgenol 42:404-10.l Daland, E.M. (1941) Surgical treatment of postirradiation necrosis. Am J Roentgenol 46:287-301.l Galler C, Epstein J, Guze K, et al. (1992) The development of osteoradionecrosis from sites of periodontal disease activity: Report of 3 cases. J Periodontol 63:310-16.l Chang D, Sandow P, Morris C, et al. (2007) Do pre-radiation extractions reduce the risk of osteoradionecrosis of the mandible. Head and Neck 29:528-36.l Beumer J, Harrison R., Sanders B., Kurrasch M. (1983a) Preradiation dental extractions and the incidence of bone necrosis. Head and Neck Surg 5:514-21.l Starcke E, Shannon I. (1977) How critical is the interval between extractions and irradiation in patients with head and neck malignancy. Oral Surg Oral Med Oral Path. 54:333-7.
- 54. Referencesl Rothwill B. (1987) Prevention and treatment of the orofacial complications of radiotherapy. J Am Dent Assoc 114:316-22.l Mealy B, Semba S, Hallman W. (1994) The head and neck radiotherapy patient: Part 2 –Management of oral complications. Compend Contin Educ Dent 14:442-52.l Oh H-K, Chambers M, Garden A et al. (2004) Risk of osteoradionecrosis after extraction of impacted third molars in irradiated head and cancer patients. J Oral Maxillofac Surg 62:139-44.l Kasibhatla M, Kirkpatrick J, Brizel D. (2007) How much radiation is the chemotherapy worth in advanced head and neck cancer. Int J Radiat Oncol Biol Phys 68:1491-5.l Fowler JF. (2008) Correction to Kasibhatla et al. How much radiation is the chemotherapy worth in advanced head and neck cancer. Int J Radiat Oncol Phys 71:326-9.
- 55. The End


 Restoration of Posterior Quadrants and Treatment Planning
Restoration of Posterior Quadrants and Treatment Planning
 Single Tooth Defects in Posterior Quadrants
Single Tooth Defects in Posterior Quadrants
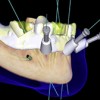 Computer Guided Treatment Planning and Surgery
Computer Guided Treatment Planning and Surgery
 Cement Retention vs Screw Retention
Cement Retention vs Screw Retention
