This lecture discusses the current methods used to restore acquired and congenital ear defects. Topics covered include surgical alterations during resection of ear tumors that enhance the prosthetic prognosis, and a detailed description of the methods used to fabricate ear prostheses including making impressions, sculpting and margin placement, flasking and processing, and coloration. The lecture concludes with a detailed discussion of the use of craniofacial implants used for retention including implant connecting bar design, and management of implant related complications.
Maxillofacial Prosthetics – Restoration of Ear Defects – Course Transcript
- 1. Restoration of Ear Defects John Beumer III DDS, MS Don Pedroche DDS, CDT Division of Advanced Prosthodontics UCLA School of Dentistry*The material in this program of instruction is protected by copyright ©. Nopart of this program of instruction may be reproduced, recorded, ortransmitted by any means, electronic,digital, photographic, mechanical, etc.or by any information storage or retrieval system, without prior permission.
- 2. Table of Contentsl Alterations at surgery to enhance the prosthetic prognosisl Etiologyl Presurgical Consultationl Master impressionsl Sculpting and margin placementl Processing the silicone prosthesisl Colorationl Partial ear defectsl Craniofacial Implants
- 3. Alterations at surgery to enhance the prosthetic prognosisEar defects v Total auriculectomy defects are easier to restore than partial auriculectomy defects v Retain the tragus v Line the defect with a split thickness skin graft v Avoid the use of flaps with hair follicles v When appropriate, place osseointegrated implants
- 4. a Alterations at surgery to enhance the prosthetic prognosis Unfavorable ear defectsLarge displaced ear fragments. Bilateral symmetry withopposite ear cannot be achieved with the prosthesis
- 5. Alterations at surgery to enhance the prosthetic prognosis Unfavorable ear defectsPartial ear defects are more difficult to restore because: v Blending margins is more difficult v Bilateral symmetry may be impossible to restore
- 6. Alterations at surgery to enhance the prosthetic prognosisv Retain the tragus.v Line site with split thickness skin graft. Why?The tragus helps hide the anterior margin of the prosthesis
- 7. Alterations at surgery to enhance the prosthetic prognosis Unfavorable ear defectsThis defect has been lined with a hair bearing scalp flap.Problems that result:v Difficult to use skin adhesivesv We are unable to place osseointegrated implants through skin with hair follicles. Why?
- 8. Alterations at surgery to enhance the prosthetic prognosis Unfavorable ear defectsSebaceous secretions from the hair follicles adhere to thesurface of the implant abutments and the implant connectingbar. These secretions become contaminated with bacteriaresulting in constant tissue irritation of the peri-implant tissues.
- 9. Alterations at surgery to enhance the prosthetic prognosisv Whenappropriate, place osseointegrated implants v Treatment time is reducedv Caution v Ifthe patient is scheduled to receive postoperative radiation one may wish to reconsider, particularly if the dose will be above 65 Gy. The backscatter will enhance the dose delivered to the bone anchoring the implant 15-18 percent (see lecture entitled “Implants in irradiated tissues.”
- 10. Restoration of Ear DefectsA difficult challenge. Both surgicalreconstruction and prostheticrehabilitation have distinct limitationsv The surgeon is limited by the complexity of the structures to be reconstructed, the availability of tissue, compromise of the local vascular bed by radiation in tumor patients and the need for visual inspection of oncologic defectsv The prosthodontist is limited by the properties of the available materials , mobility of the tissues Surgically adjacent to the defects. reconstructed ear
- 11. Etiologyv Facial neoplasms v Basal cell carcinoma v Squamous carcinoma v Malignant melanomav Craniofacial anomalies v Microtiav Trauma v Burns
- 12. Ear prosthesisPreop consultation and impression
- 13. Presurgical ConsultationIssues v Psychosocial v Impressions v Photographs v Explain the limits of the prosthetic rehabilitation v Brief review of prosthetic care procedures
- 14. Presurgical ConsultationPsychosocial issues v Challenges confronting tumor patients v Mortality v Morbidity v Functional impairments v Esthetics v Quality of life – Social function v Challenges confronting the provider v Establish lines of communication v Maintain empathy and compassion while at the same time maintaining the ability to motivate the patient to perform needed home care procedures
- 15. Presurgical ConsultationTasks to be accomplished a) Impressions and photographs b) Patient education regards nature of the defect and the purpose of the prosthesis c) Patient expectations need to tempered
- 16. Master impressions v Irreversiblehydrocolloid v Light body polysulfide v Light body polysiloxane v Digital impression techniquesThe objective is to obtain an impression withoutdisplacing tissues
- 17. CAD-CAM Techniquesa b c dWax patterns can be developed with CAD-CAMtechniques a: Normal ear opposite the defect. b: 3D image of normal ear. c: Mirror image of normal ear. d: Wax pattern developed from mirror image data.
- 18. Sculpting and margin placement A selection of wax ears can be accumulated by making an extra casting from every impression.Dividing normal ear into equal compartments will aid sculpting.Note how anterior margin is feathered.
- 19. Sculpting and margin placement The wax sculpting of the ear is positioned on the patient. The sculpture is checked for contour, symmetry with opposite ear and margin placement.
- 20. Margin placementa bv The anterior margin is thinned and placed behind the tragus if this structure is present (a)v If the tragus is absent the anterior margin is thinned and blended into the skin (b)
- 21. Surface textureA moderate stipple is used to reproduce the surfacetexture of the adjacent skin and opposite ear.
- 22. Processing the silicone prosthesis Investing and flaskingA three piece mold is made to facilitate removal of thesilicone casting from the mold after processing
- 23. Intrinsic coloration Base ShadeLightest skin shade is selected favoring the yellow tones
- 24. Coloration Surface Detail – Intrinsic vs ExtrinsicWe prefer extrinsic coloration to create and highlight thesurface detail because:v It is easier as opposed to intrinsic coloration methodsv More consistent esthetic results can be obtained with this methodv This method is more time efficient. Multiple prostheses can be efficiently fabricated with this technique
- 25. ProcessingThe silicone is mixed, vacuumed to eliminate airbubbles, and injected into the mold. Followingpolymerization, the ear casting is removed.
- 26. Extrinsic coloration
- 27. Coloration – Extrinsic v Shade guides will ensure consistency in color and translucence of base. v Coloration is accomplished under corrected light conditions.
- 28. Deglossing.a b cAdding small amounts of fumed silicone dioxide (Cabo-O-Sil) to the RTVsilicone used for sealing will moderate some of the shine. Care should betaken to avoid applying excessive thickness of sealant. Excessive shinecan also be avoided by using a dry brush as a blotter as the siliconebegins to cure after applying the initial layer of sealant. This process isrepeated twice at 5 minute intervals upon application of the siliconesealant. The purpose of this technique is to maintain the original surfacetexture and avoid excessive shine.
- 29. Deglossing.a b ca : Before deglossing and after sealant applied.b : After deglossing.c : Prosthesis in position.
- 30. Coloration – Extrinsic Finished ear prostheses. Note excellent color matching, surface texture reproduction and marginal adaptation.v Tragus hides some of the anterior marginv Without a tragus the margin anteriorly is carefully thinnedv Ear lobe margins represented by a line in the skin
- 31. Partial ear defectsv Small ear defect.v Prosthesis engages undercuts behind ear and in concha to enhance retention.v Margins are strategically placed and carefully thinned and adapted
- 32. Partial ear defectsv Small ear defect.v Prosthesis is implant retained.v Exposed margins are carefully thinned and adaptedNote: Partial ear prostheses are only effectivewhen the remaining ear fragment is not displaced.
- 33. Use of Craniofacial Implants to Restore Auricular DefectsFor many years we have been able to produce exceptionalesthetic resultsChallenges:v Patient acceptancev Retention
- 34. Use of Craniofacial Implants to Restore Auricular Defects Benefits(1) Improved retention and stability of the prosthesis(2) Elimination of occasional skin reaction to adhesives(3) Ease and enhanced accuracy of prosthesis placement(4) Improved skin hygiene and patient comfort(5) Decreased daily maintenance associated with removal and reapplication of skin adhesives(6) Increased life span of the facial restoration (when skin adhesives are used for retention, they must be removed and reapplied each day, leading to loss of colorants at the margin of the prosthesis and eventually rendering the prosthesis unacceptable)(7) Enhanced esthetics of the lines of juncture between the prosthesis and skin. When an implant-borne prosthesis is fabricated its margins can be made thinner and positive pressure can be developed by the margins of the prosthesis with the movable peripheral tissues.
- 35. Facial Prostheses – Retention During Daily Activities Adhesive Implant 100 95 * 89 84 * 85 79 * 80 63 % Excellent 57 60 44 44 38 40 20 0 Home Eating Exercise Perspire Sneeze/CoughChang et al, 2005
- 36. Frequency of Wear Facial Prostheses Adhesive Implant Chang et al, 2005 120 95 100 100 89 88% Wearing 80 63 * 60 44 40 20 3 0 0 Home Work Social Never
- 37. Ear Implants-Treatment Planning CT Scan-Bone quantity Markers Two to three implants areRadiographic Stent placed posterior and superior to the ear canal
- 38. Congenital ear defectsIn patients with congenital ear defects the major issue is the fate of tissueremnants. With microtia ear remnants will vary in size, shape and positionand may need to be removed. Before these remnants are resected allpossible options for habilitation must be presented, explored anddiscussed with the patient and their family. In some patients it may bedesirable to reconstruct the ear canal. If so, this procedure can beperformed during the same surgery as implant placement.
- 39. Congenital ear defectsa: Patient presented with microtia. Attempts were made toreconstruct the auricle, but the results were unsatisfactory.The reconstructed ear was removed and implants placed.b and c: Surgical template was used to help properly positionimplants.
- 40. Surgical templatesA preliminary wax sculpting is fitted to the patient, themost desirable implant positions are identified and asurgical template is designed to enable accuratepositioning of the implants.
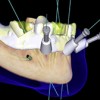
- 41. Craniofacial implantsv Implants 4mm or 5mm in length are used. Note the flange design.v The flange prevents impaction of the implant intra-craniallyv Two to three implants are placed posterior and superior to the ear canal
- 42. Implant placementa b c d ef g h iImplant placement in mastoid bone. a: Auricular defect. b: Waxsculpting fitted to identify proper implant position. c: Surgicaltemplate. d: Flap reflected. e and f: Template used to locateproper implant positions. g: Mastoid exposed and sites prepared forthree implants. Note countersink. h: Implant fixtures placed intoprepared sites. i: Wound closed in three layers.
- 43. Ear Implants-Soft Tissue ConsiderationsAt second stage surgery care is Purpose: Reduce the lengthtaken to thin the tissue flap of the peri-implant pocketsoverlying the implant sites
- 44. Auricular Implants-Soft Tissue Considerations The skin around these sites is almost completely healed 4 weeks after second stage surgery.These implants emerge through a split thickness skin graft that had beenplaced previously. The granulation tissue (arrow) is secondary to keratinbuildup and accumulations of sebaceous secretions. The implant surfaces must be kept clean if peri-implant tissues are to remain healthy.
- 45. Prosthetic Techniques Impressionsa b c d e fa: Impression copings are secured to implant fixtures.b: Thin layer of rubber base impression material applied.c: Thin layer of gauze imbedded in impression material.d: Plaster backing.e: Impression with abutment analogues attached.f: Master cast.
- 46. Prosthetic Techniques Fabrication of implant connecting bara b c da: Wax sculpture positioned on master cast.b: Silicone template fabricated as an aid to fabricate tissue bar.c: Pattern for tissue bar. In this case, implants were positionedperfectly.d: Completed implant connecting bar
- 47. Prosthetic TechniquesAcrylic resin substructure to be imbedded withinsilicone prosthesis. It contains retentive elements.
- 48. Prosthetic Techniques a ba: Extrinsic coloration added to silicone prosthesis.b: Clips placed into substructure.
- 49. Metal framework must fit passivelyBoth of these patients rely primarily on the Haderbar and clip system for retention of their prostheses
- 50. Auricular Implants – Bar DesignsThese patients rely primarily on the Hader barand clip system for retention of their prostheses
- 51. Completed Prosthesis in Position
- 52. Individual attachments Zest anchorsAdvantages ” Easier to use ” Quicker and less expensive than an implant connecting bar
- 53. Individual Attachments We no longer use them. Why? Retention is adequate, but stability is suboptimal and we have had a higher rate of failure with these systemsWe recommend that craniofacial implants be splintedtogether with a bar for best long term results.
- 54. Implants in the mastoid (UCLA Data – Followup: 4 – 13 years) Defects Patients #placed #failed #buried Success rateTumor 13 35 1 3 93.3%Congenital 12 47 4 2 87.2%Trauma 11 35 0 9 100%Totals 36 117 5* 9 91.5%3 of the 5 failures were due to trauma (a blow to the head). Overallsuccess rate without the loss of these 3 implants would be 95%
- 55. Craniofacial Implants Placed in the Mastoid to Retain Ear Prostheses Soft Tissue Response Grade #Visits/Site 0 60 1 32 2 5 3 3 4 1 Total 101
- 56. Soft Tissue ResponseModerate Erythema Erythema withGrade 1 supporation Grade 4
- 57. Soft Tissue ResponseTreatment – Improve hygiene
- 58. Soft Tissue Responsev Patient suffered from persistent soft tissue irritation. All conservative measures failed including a course of systemic antibiotics based on culture.v Porcelain added to transcutaneous portion resolved tissue irritation.
- 59. Irradiated sitesv Tissue bar with magnetic retention in irradiated patient. Note flange exposures. Two of three implants were lost.v In irradiated sites most implant failures are after loading.
- 60. Irradiated Sites Irradiated sites v An osteoradionecrosis associated with implants v Patient was treated with 60 Gy v Following removal of the implant the exposed bone sequestrated followed by complete healing
- 61. v Visitffofr.org for hundreds of additional lectures on Complete Dentures, Implant Dentistry, Removable Partial Dentures, Esthetic Dentistry and Maxillofacial Prosthetics.v The lectures are free and available upon registering for the sitev Our objective is to create the best and most comprehensive online programs of instruction in Prosthodontics


 Implants and RPDs
Implants and RPDs
 Restoration of Posterior Quadrants and Treatment Planning
Restoration of Posterior Quadrants and Treatment Planning
 Prosthodontic Procedures and Complications
Prosthodontic Procedures and Complications
 Computer Guided Treatment Planning and Surgery
Computer Guided Treatment Planning and Surgery
