This lecture discusses the role of the prosthodontist in the care of patients born with cleft lip and palate. Topics covered include facial and palatal development, the
epidemiology of cleft lip and palate, naso-alveolar molding, methods used in surgical repair, fabrication of overlay removable partial dentures and complete dentures, and the use of osseointegrated implants including zygomaticus implants to retain overdentures and overlay removable partial dentures.
Maxillofacial Prosthetics – Cleft Lip and Palate – Course Transcript
- 1. Restoration of Cleft Lip and Palate Arun Sharma DDS Department of Preventive and Restorative Dentistry, UCSF John Beumer III, DDS, MS Ting Ling Chang, DDS Division of Advanced Prosthodontics, UCLA*The material in this program of instruction is protected by copyright ©. Nopart of this program of instruction may be produced, recorded, ortransmitted by any means, electronic,digital, photographic, mechanical etc.or by any information storage or retrieval system, without prior permission.
- 2. Table of Contentsv Facial and palatal developmentv Classification of cleftsv Incidencev Etiologyv Early intervention and counselingv Lip repairv Palatal repairv Growth and development and orthodontic treatment v Arch expansion eruption of teeth v Cuspid substitution
- 3. Table of Contentsv Adjunctive surgical procedures v Orthognathic surgery v Pharyngeal flap v Nasal revisionv Role of obturator prosthesis in childrenv Closing oronasal fistulas and grafting the cleftv Stabilizing non-grafted cleft segmentsv Replacing the missing lateral incisorv Complete dentures v Role of osseointegrated implantsv Zygomaticus implants for cleftsv Overlay removable partial dentures v Role of osseointegrated implants
- 4. Development of Facial Structures Drawings depicting the formation of the face from the frontal perspective from the fourth week through the eighth week.From Patten, B. M., 1969
- 5. Development of Facial Structures Drawings depicting the formation of the face from the frontal perspective from the fourth week through the eighth week.From Patten, B. M., 1969
- 6. Development of Facial Structures Drawings depicting the formation of the face from the frontal perspective from the fourth week through the eighth week.From Patten, B. M., 1969
- 7. Development of Facial Structures Drawings depicting the formation of the face from the frontal perspective from the fourth week through the eighth week.From Patten, B. M., 1969
- 8. Development of Facial Structures Drawings depicting the formation of the face from the frontal perspective from the fourth week through the eighth week.From Patten, B. M., 1969
- 9. Cleft lip and palate Diagnosis v Prenatal Ultrasound Cleft
- 10. Development of Facial Structures A. Median nasal process B. Lateral nasal process C. Maxillary process
- 11. Palatal Development” Palatogenesis begins 5th week” Completed by the 12th week Develops from two primordia: The primary palate The secondary palates
- 12. Development of the Palate Section of the head of the embryo late in the eighth weekFrom Patten, B. M., 1969
- 13. Palatal Development Graphic summary of palatal fusion from the 6th week to the 9th week.From Patten, B. M., 1969
- 14. Palatal Development Graphic summary of palatal fusion from the 6th week to the 9th week.From Patten, B. M., 1969
- 15. Palatal Development Graphic summary of palatal fusion from the 6th week to the 9th week.From Patten, B. M., 1969
- 16. Palatal Development Graphic summary of palatal fusion from the 6th week to the 9th week.From Patten, B. M., 1969
- 17. Palatal Development Graphic summary of palatal fusion from the 6th week to the 9th week.From Patten, B. M., 1969
- 18. Palatal Development Graphic summary of palatal fusion from the 6th week to the 9th week.From Patten, B. M., 1969
- 19. Palatal Development Graphic summary of palatal fusion from the 6th week to the 9th week.From Patten, B. M., 1969
- 20. Classification of Clefts v Cleft lip and alveolus (primary palate) v Cleft of the hard and soft palate (secondary palate) v Combinations of these twov Clefts can be bilateral or unilateralv Embryologically, anterior clefts differ from posterior clefts
- 21. Classification of CleftsCleft patients may also present with other abnormalities” Syndromic forms (15%)” Nonsyndromic forms (85%)
- 22. Possible combinations of Cleft Lip and Palate
- 23. Incidence of Clefting ” 1 in 700 infants born ” Left sided clefts account for 70%Highest rates in American Indians (1 in 278births) followed by the Japanese, Maoris,Chinese, Caucasians and African Americans(1 in 3,330 births).
- 24. IncidenceCleft lip (with or without cleft palate) ” One in every 1000 births ” Males affected twice as frequently as females
- 25. Incidence Cleft Palate (with or without Cleft Lip)” With or without cleft lip, occurs once in 2500 births” Isolated clefts of the palate are more common in females* *May be due to the fact that the palatine processes fuse about 1 week later in females than in males.
- 26. Etiology v Geneticfactors v Environmental factors affecting the mother during the first trimester v Infection v Hormonal imbalances v Poor diet v Teratogenic agents**Ethanol, folate antagonists, alkylating agents, phenytoin, trimethadione,valproic acid, benzodiazepines, meprobamate, barbiturates
- 27. Treatment SequenceLip repairPalatal repairOrthodontic treatmentSecondary surgical procedures Pharyngeal flaps Bone grafting the cleft Repairing the nasal deformity Orthognathic surgeryReplacing the missing dentition
- 28. Treatment Sequence
- 29. Early Intervention and Counseling” Cleft team members assist with the emotionaland social adjustment of the family” Before leaving the hospital parents should beable to feed the infant and examine and clean thecleft
- 30. FeedingA variety of feeding aids have been developed toaid in feeding the cleft infant.
- 31. Genetic Evaluationv Parental history v Exposure to teratogensv Family history v Relativeswith a cleft, lip pits, mental retardation, congenital heart disease, limb and ocular disordersv Syndromic conditionsv Chromosomal analysis
- 32. Team EvaluationTeams are usually comprised of an audiologist,geneticist, genetic counselor, nursecoordinator, oral and maxillofacial surgeon,orthodontist, otolaryngologist, pediatrician,pedodontist, plastic surgeon, prosthodontist,speech pathologist, and social worker.
- 33. Role of Prosthodontistv Nasoalveolar moldingv Interim obturators/speech aidsv Management of edentulous spacesv Tx planning restorations for missing teeth and correction of tooth size discrepanciesv Unrepaired cleft palates
- 34. Current protocol for most major cleft palate teamsEarly counseling –prenatal/feedingTaping or naso-alveolar molding (NAM)Lip repairPalate repairSpeech therapyPharyngeal flapOrthodonticsAlveolar cleft graftOrthognathic surgeryReplacing missing teethLip and nose revision
- 35. Presurgical Infant Orthopedic Appliance (PSIO)l McNeil 1950, Mylin 1968, Latham 1980l To move the alveolar segments closer together
- 36. Nasoalveolar Molding Appliance (NAM)v Reduce the size of the intraoral alveolar cleftv Mold and position the surrounding soft tissues including the deformed soft tissue and cartilage in the cleft nose.v Tissue expansion – Columella
- 37. Nasoalveolar Molding Protocol (Grayson et al, 2001)Early intervention <1mLabor intensive 1-2hrs/wk x 12-24wksBilateral cleft Need 5-6mths moldingUnilateral cleft Need 3mths moldingv Alveolar or nasoalveolar molding from birth to 12 wksv 12-14 wks primary cleft lip repair, nasal, and GPP (gingivoperiosteoplasty) in one stage
- 38. Nasoalveolar Molding Appliance (NAM)ResultØ Overall improvement in the esthetics of the naso-labial complex – Less scarringØ Minimize the extent of surgery and the overall number of surgical procedures
- 39. Nasoalveolar Molding Appliance (NAM) Impressions and castsa b c a. During impression, infant’s head must in an upright position and well supported. b. Impression of silicone putty. c. Master cast.
- 40. Fabrication of the oral portion of NAM appliance l Cast made from the master cast-wax blockout. l Oral portion of PNAM device made of clear acrylic resin. l Completed device on altered cast. Note posterior extension. Excessive length in this area will precipitate gagging.
- 41. Fabrication of the oral portion of NAM appliance Clear acrylic resin Fill the cleft region of the palate and alveolus to approximate the contour & topography of an intact arch
- 42. Fabrication of the oral portion of NAM appliancel Diagrammatic representation of the subtractions and additions made to NAM device in unilateral cleft.
- 43. Fabrication of the oral portion of NAM appliance v Fill in cleft with wax v Restore palatal contours v Duplicate cast
- 44. Fabrication of the oral portion of NAM appliance v All tissue border must be smooth v Proper contour and finish for tongue space v Limit posterior extension to avoid gagging
- 45. Unilateral clefts Oral molding portion plus nasal extensionHow to retain the oral Adhesive tapemolding appliance? & elastics
- 46. Unilateral clefts Oral molding portion plus nasal extensionv The nasal extension serves as a custom tissue expander to correct the flattening nasal deformity It also brings the columella into a more midline position.v Adjustments and additions are performed weeklyv Note the molding of the nasal cartilage. This projection is formed chair side with temporary denture reline materials
- 47. Unilateral clefts Oral molding portion plus nasal extensionv Nasoalveolar molding is nearly complete. The columella is approaching midline and the nostril on the cleft side is becoming more symmetrical.v It usually takes 4-6 weeks to attain proper alignment of the alveolar cleft segments. At 3 months most patients are ready for surgery
- 48. Bilateral cleftsv In addition to realigning cleft segments a principle advantage of NAM in bilateral clefts is elongation of the columella for this often eliminates the need for further surgery to elongate this structure.v NAM of bilateral clefts consists of three stages v Repositioning the posterior palatal segments and rotating the premaxilla into position v Repositioning the alar cartilages v Lengthening the columella
- 49. Bilateral cleftsv Nasoalveolar molding device for bilateral cleft. Nasal extensions in position.v In bilateral clefts, when the premaxilla attains a reasonable position, nasal molding begins. The tips of the nasal extension should be kept close together. Otherwise the tip of the nose and the columella will be excessively widened.
- 50. Bilateral cleftsv As the position and contours of the nose and nasal cartilages become more normal, elongation of the columella begins. A horizontal strip of soft acrylic resin, the so-called prolabial band, is secured to the two nasal extensions. The prolabial band cinches the columella and provides length rather than width to the columella.v This method, when effectively employed, will lengthen the columella by 4-7 mm.
- 51. Bilateral cleftsAvoid excessive pressure at the lip columellajunction. Doing so may result in ulceration ofthis area, compromising the final result.
- 52. Before and after NAMThe patient is now ready for surgery. Itusually takes 5-6 months before the tissuesare optimized and the patient is ready forsurgery.For details see: Brecht L. “Nasoalveolar Molding” in MaxillofacialRehabilitation: Prosthodontic and Surgical Management of Cancer-related,Acquired and Congenital Defects of the Head and Neck. Eds. Beumer J,Marunick M, Esposito S. Quintessence Pub Co. Chicago, IL, 2011 pp 324-9
- 53. Surgical Treatment – Lip RepairRule of tens: Lip is repaired* when the patient is 10 weeks old, 10 pounds in weight, with a hemoglobin count of 10. *The first surgery is usually performed at about 3 months. This period may be extended to complete NAM, particularly in patients with bilateral clefts.
- 54. Surgical Treatment – Lip Repair A B CModified Le Mesurier surgical technique for lip closure.A: Development of flaps. B: Flaps prepared forclosure. C: Lip closure.*Methods of closure were developed based on the nature of thecleft, the deficiency of the tissues associated with the cleft, andconsequences of scar contracture.
- 55. Surgical Treatment – Lip Repair Unilateral cleftAfter lip repair. Note the nasal asymetry. The scarring fromthe closure of the lip and cleft will impair the development ofnormal nasal contours and will probably require correction inthe future.
- 56. Surgical Treatment – Lip Repair Bilateral cleftAfter lip repair. Note the short columella. The scarring fromthe closure of the lip and cleft will impair the development ofnormal nasal contours and will require correction in the future.
- 57. Complications associated with lip repairv Multiple additional surgeriesv Less than ideal esthetic result v Notethe excessive scarring associated with this lip closure of a bilateral cleft
- 58. Surgical Treatment – Palatal Repair Timing – Approximately 10 months Methods of closure vary depending upon: v Extent of the cleft v Availability of tissue v Experience of the surgical team Palatal pushback procedure
- 59. Surgical Treatment – Palatal RepairTiming of closure is a matter of opinion. Twopositions:” Delayed closure (Zurich approach) – Less inhibition of maxillary growth” Early closure – Better speech patterns develop early Palatal push back and closure procedure
- 60. Complications associated with palatal repairv Shortsoft palate resulting in velopharyngeal insufficiency. Speech will be hypernasal.
- 61. Growth and DevelopmentGrowth may be inhibited by:v Intrinsictissue deficienciesv Quality, amount and location of scar tissue secondary to the surgical repairs
- 62. Growth during primary and mixed dentition stageComplicating factors 1. Tight lip 2. Scar tissue bands in the palate These phenomenon result in a deficiency in the downward and forward growth of the maxilla because of impaired alveolar development.
- 63. Growth and DevelopmentOrthodontic treatment – Purposes:v Expand the maxilla to correct segment position and crossbitev Monitor eruption of teeth Treatment begins during the mixed dentition stage.
- 64. Growth and Development Orthodontic treatment Patient with a repaired unilateral cleft. Note the arch expansion after one year.It is vitally important that the maxillary fragments not be allowed to collapsemedially. If they do the tongue will rest on the dentition preventing furtherdevelopment of the maxilla and impair alveolar development.
- 65. Growth and Development Orthodontic treatment – Other considerations ” Should the missing lateral incisor space be kept open for prosthetic replacement with an implant supported restoration or closed by eruption and medial movement of the cuspid.Choice depends upon:” Size and shape of the cuspid and the size of the maxilla.” If it is decided that the cuspid should come forward, the cleft is grafted afterarch expansion but before the cuspid has moved down into the bony defect.
- 66. Growth and Development Orthodontic treatment – Other considerations ” Should the missing lateral incisor space be kept open for prosthetic replacement with an implant supported restoration or closed by medial eruption and movement of the cuspid.v Bilateral clefts we favor canine substitution.v Unilateral clefts we tend to create space orthodontically for placement of an implant
- 67. Growth and development during adolescencev Progressive retrusiveness of the maxilla may occur during later growth.v The tight lip scar and scar tissue bands in the palate impede the forward growth of the maxilla as well as the alveolar processes
- 68. Adjunctive Surgical procedures Orthognathic SurgeryAs a result many cleft patient require a maxillaryosteotomy to bring the maxilla down and forward.
- 69. Pharyngeal Flapsv Mostvelopharyngeal discrepancies for cleft patients aremanaged surgically, usually with a combination of a palatalpush back and closure procedure (9-18 months).v However in a small percentage of patients, a superiorly basedpharyngeal flap (3-7 years) is required to enable the patient toachieve velopharyngeal closure. Superiorly based pharyngeal flap.
- 70. Pharyngeal Flapsv Flaps are raised on the nasal surface of soft palate and from the pharyngeal wall. The pharyngeal flap is rotated onto the soft palate as shown.v As organization and contracture occurs, the soft palate is pulled toward the area of normal closure. Superiorly based pharyngeal flap.
- 71. Pharyngeal Flaps” Closure of the lateral portals is accomplished by contracture of lateral pharyngeal walls.” Today only a small percentage of patients require flaps Superiorly based pharyngeal flap.
- 72. Adjunctive Surgical procedures Correcting nasal deformitiesObjectives” Lengthen the columella” Correct deficiencies associated with the nasal cartilage on the cleft side” Develop proper contours of the nasal tip
- 73. Adjunctive Surgical procedures Correcting nasal deformitiesObjectives” Lengthen the columella” Correct deficiencies associated with the nasal cartilage on the cleft side” Develop proper contours of the nasal tip This patient has a rather typical result after nasal revision surgery
- 74. Adjunctive Surgical procedures Correcting lip deficienciesContour deficiency often occur secondary to scarringassociated with closure. Note the corrections madein the length of the lip, the lip line and contour.
- 75. Adjunctive Surgical procedures Correcting lip deficiencies Contour and tissue deficiencies occasionally occur secondary to scarring associated with closureLip switch (Abbey flap) ” In this procedure a pedicle flap from the lower lip is used to provide more tissue for the upper lip.
- 76. Adjunctive Surgical procedures Lip switch (Abbey flap)A typical result. Note the scar on the lower lip
- 77. Role of Obturator Prosthesis in Childrenv Clefts of the secondary palate with a paucity of residual palatal tissuesv Poor anesthetic risksv Failed pharyngeal flaps
- 78. Role of Obturator Prosthesis in Children Very short soft palates following surgical repair The repaired soft palate is quite short in both of these patients and cannot reach and engage the posterior pharyngeal wall during velopharyngeal closure. As a result speech will be hypernasal and swallowing will be impaired.
- 79. Role of Obturator Prosthesis in ChildrenFailed pharyngeal flap. Why has it failed to restorespeech? The pharyngeal flap is too low to effectively interact with the lateral pharyngeal walls during velopharyngeal closure. As a result speech is hypernasal.
- 80. Interim Speech AidsSoft palate obturators are fabricated in the usual fashion (see “Restoration of Soft Palate Defects” FFOFR.org) v Fabricate palatal stent with adequate retention. v Gradually develop the pharyngeal extension. v When the child is has accommodated to the pharyngeal extension, develop the obturator portion.
- 81. Interim Speech Aids The bulb is molded with compound and thermoplastic wax.v The extensions of the prosthesis aredeveloped with dental compound and athermoplastic waxv Following processing the contoursand extensions are verified withpressure indicating paste and/ordisclosing wax (see “Restoration of softpalate defects” FFOFR.org for details).
- 82. Interim Speech Aids A completed speech bulbObturator prostheses restore velopharyngeal function veryeffectively and are well tolerated by the patient. They needto be remade periodically to account for growth and eruptionof the permanent dentition.
- 83. Obturator prosthesisfor failed pharyngeal flaps Obturators for failed pharyngeal flaps are rarely successful because it is difficult to extend the prosthesis superiorly to engage the movable lateral pharyngeal walls.
- 84. Obturator prosthesis for failed pharyngeal flapsIn this patient, the bulb resulted in constant contact with non-mobile pharyngeal tissues, resulting in hyponasal speech.The bulb was discarded and the flap removed. Velopharyngeal function and normal speech was eventually restored with a new obturator prosthesis after the flap had been removed.
- 85. Stabilizing the cleft segments after orthodontic treatmentFollowing orthodontic carerapid relapse and archcollapse occurs if the cleftsare not rigidly secured.This relapse is primarilydue to the stretching of themidline scar secondary tosurgical closure of the cleft. Since the 1950’s two methods have been used: v Fixed partial dentures (1950 – mid 1970’s) v Autogenous bone grafts (mid 1970’s – present)
- 86. Bone Grafting the CleftGoals for grafting the cleftv To separate the oral and nasal cavitiesv To stabilize the maxillary segments with a bony unionv To provide normal quality of bone in the alveolus for orthodontic movement and support of teethv To provide adequate 3 dimensional bone volume for placement of osseointegrated implants
- 87. Bone Grafting the CleftTiming of graftingv Mixed dentition stage is preferred by most teamsv Early grafting (during infancy) of the cleft may have a negative affect on the growth of the maxilla
- 88. Closing oronasal fistulas and grafting the cleft Graft materialNasal mucosa lining aswell as oral mucosal liningis required to enclose thegraft material.
- 89. Stabilizing non-grafted cleft segmentsFixed partial dentures – From the 50’s thru the mid 70’s the maxillaryfragments were often stabilized with fixed partial dentures.Full veneer crowns wererequired to maximize retention.Two abutments or more in eachcleft segment is recommended.
- 90. Stabilizing non-grafted cleft segments Fixed partial dentures – From the 50’s thru the mid 70’s the maxillary fragments were often stabilized with fixed partial dentures.In this patient partial veneer crowns were sufficient.Two abutments were used in each cleft segment.
- 91. Stabilizing non-grafted cleft segmentsFixed partial dentures – From the 50’s thru the mid 70’sthe maxillary fragments were often stabilized with fixed partialdentures. In this patient partial veneer crowns were sufficient. Double abutments were used in each cleft segment.
- 92. Restoring the missing and malformed dentition Dental discrepancies of patients with cleftsv Missing lateral incisors (40%)v Maxillary central adjacent to the cleft is often undersizedv Teeth in the premaxilla have shortened rootsv 24% have missing premolarsv More likely to possess super- nummery teeth (21%)v Teeth adjacent to cleft often present with hypocalcified enamelv Hypodontia (50%)
- 93. Replacing the Missing Lateral IncisorImplants – Issues ” Growth – Skeletal Development “ Dental alveolar “ Mandible and maxilla “ It is advisable to wait until two consecutive cephalometric films one year apart show no evidence of growth ” Site development “ Horizontal and vertical deficiencies usually present
- 94. Replacing the Missing Lateral Incisor Cuspid substitution vs implantsv Bilateral clefts we favor canine substitution.v Unilateral clefts we tend to create space orthodontically for placement of an implant
- 95. Replacing the missing lateral incisor Removable Partial Dentures A rotational path of insertion RPD was used to replace the lateral incisor.
- 96. Replacing the missing lateral incisor ImplantsIssues” Consequences of premature placement “ Implant will be submerged relative to the adjacent teeth with the attendant esthetic consequences “ Less favorable implant biomechanics ie. crown root ratiosIn this patient with a missing lateral incisor, the implant was placed prior to thecompletion of growth. As the adjacent natural dentition continued to erupt andthe implant crown appeared submerged relative to the adjacent teeth.
- 97. Replacing the missing lateral incisor ImplantsIssues” Consequences of premature placement “ Implant will be submerged relative to the adjacent teeth with the attendant esthetic consequences “ Less favorable implant biomechanics ie. crown root ratiosSee “Implants in Growing Children” FFOFR.org for details
- 98. Replacing the missing lateral incisor Implants At age 21 the implant crown was replaced. Note the discrepancies associated with the the gingival levels of the lateral incisors.
- 99. Replacing the Missing Lateral IncisorImplants – Issuesv Gingival contours are not quite normalWhy? Scarring associated with the closure and grafting the cleftConsequences: None. Almost all cleft patients have a low smile line.
- 100. Replacing the Missing Lateral IncisorNote gingival contours.These are to be expected giventhe scarring secondary to themultiple surgical proceduresnecessary to close and graft thecleft. UCSF Data (Sharma and Vargervik, 2006) ” 24 patients (15 male, 9 ” 33 implants placed female) ” 31 implants restored ” 9 bilateral clefts ” 28 still in function ” 15 unilateral clefts
- 101. Replacing the Missing Lateral Incisor Grafting the Cleft and Placing Implants Average age in years (UCSF data)” Alveolar cleft bone graft – 14.3 “ Range (12 – 26) Median 15″ Implant Placement – 18.1 “ Range (14 – 28) Median 19
- 102. Replacing the Missing Lateral IncisorMost clefts present with either horizontal or verticalbone deficiencies and require grafting prior toimplant placementImplant Placement n = 33 “ Adequate bone 15 (45.4%) ” Need for regraft 18 (54.6%)
- 103. Replacing the Missing Lateral Incisor Results v Implants placed – 33 v Implants restored – 31 v Implants in function – 28 *2 implants failed at 2nd stage *2 failed in a bilateral cleft after 4 years *1 failed in a unilateral cleft after 11 years
- 104. Replacing the Missing Lateral Incisor Follow up Time (months) “ Time since placement – 133.6 mths (Range 85 – 166. Median 130) “ Time since restored – 129 mths (Range 74 – 158, Median 121)
- 105. Complete Dentures Treatment concepts – Challenges and Difficulties” The reduced size of the denture foundation area” Excessive interarch space” Lack of a bony palate” Poor alveolar development with shallow depth of the palate” Scarring from lip closure” Scarring in the posterior palatal seal area” Presence of oro-nasal fistulas” Opposing natural dentition ” Misaligned and extruded teeth” Soft palate defect All these factors negatively impact the retention, stability and support provided the complete denture.
- 106. Complete Dentures Treatment concepts – Challenges and DifficultiesIn these three patients note:” Reduced size of denture foundation area” Large oronasal fistulas” Little or no alveolar ridges” Soft palate defect
- 107. Complete DenturesTreatment concepts – Challenges and DifficultiesIn these two patients note:v Scarring in the posterior palatal seal areav Collapsed maxillary arch segments
- 108. Complete DenturesTreatment concepts – Challenges and DifficultiesResult:v Dramatically compromised stability, retention and supportv Bilateral balance is virtually impossible to obtain if the opposing arch is dentate Most patients cannot masticate effectively with these dentures. The primary benefits are improved lip contours and esthetics, speech articulation and swallowing without nasal leakage.
- 109. Complete Dentures Making ImpressionsBorder mold with low fusing compound v Posterior palatal seal – single bead v Avoid excessive tissue displacement in heavily scarred areas v Develop the labial flange to support the lipCorrected impression v Carefully examine for small fistulae v Block out fistulae before making corrected impression v Use a polysulfide wash impression material v This material is less likely to fracture and become imbedded in undetected fistulae
- 110. Complete Dentures Vertical Dimension of Occlusionv Normal in patients with reasonable development of the alveolar processesv Interocclusal space is increased in patients with very small maxilla and little alveolar ridge heightv Since most patients present with a severe Class III jaw relationship the posterior teeth are set in crossbite and the anterior teeth arranged in an edge to edge relationship
- 111. Complete Dentures Try in appointmentEsthetics Anterior tooth display should be harmonious with lip thickness, scarring and contours.For example: A protruding lip scar can be made less conspicuous by moving the lateral incisor palatally.Making repeatable centric relation records. In patients with a very deficient maxilla it is advisable to use processed record bases.
- 112. The oral surfaces of the soft palate obturator extension must be concaveThis complete denture was made for a patient with a partiallyrepaired cleft lip and palate. Note that the anterior flange ismuch thicker than normal. Note the concave oral surface ofthe obturator extension to the posterior pharyngeal wall. Flator convex oral surfaces may cause gagging or difficulty duringswallowing
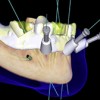
- 113. Role of Osseointegrated Implants Without the retention and stability provided by implants mastication performance is significantly degraded in edentulous patients with cleft lip and palate fitted with complete dentures. Retention and stability are particularly compromised when the prosthesis extends into the velopharyngeal region.The addition of implants can have a dramatic impact on patient function andtheir placement should be given serious consideration in all such patients.
- 114. Role of Osseointegrated Implants Patient presents with a repaired bilateral cleft of the lip and palate Note:v The premaxillary segment is missingv The cleft has not been reconstructed with a bone graftv The profound Class III jaw relation
- 115. Role of Osseointegrated Implantsv Implants have been placed into each of the remaining posteriorpalatal segments and into the anterior region of the mandible.v The remaining posterior palatal segments move independent ofone another during occlusal function and therefore it is best not toconnect one side to the other with and implant connecting bar.
- 116. Implant connecting bar designsNote:v The implant connecting bar does not cross the cleftv The bars are designed as an anterior extensionv When occlusal loads are applied anteriorly, the prosthesis rotates around the Hader attachments. The ERA attachments permits the prosthesis to be impacted into the anterior denture foundation areas.
- 117. Implant connecting bar designsBoth designs are considered implant assisted designsv In the maxilla implant support is provided posteriorly but the anterior forces are born by the edentulous denture foundation areas available for coverage and engagement.v In the mandible implant support is provide anteriorly by the implant connecting bar but posterior support is provided by the primary support areas of the mandible-the retromolar pad and the buccal shelf.
- 118. Role of Osseointegrated Implants Completed prosthesis. Note: v Crossbite v The upper lip has been reconstructed with an Abbey flap.
- 119. Role of Osseointegrated Implants v Implants were placed bilaterally v The two implants on the left failed. v Implant connecting bar was designed to provide retention and stability but they are not the primary means of support.
- 120. Zygomaticus implants for cleftsAdvantages vs sinus augmentationv Fewer surgeriesv Reduced treatment timev No donor site morbidity
- 121. Zygomaticus implants for cleftsIssues to consider during treatment planningv Generally two implants are placed on each side.v The implants are then splinted together with an implant connecting bar
- 122. Zygomaticus implants for cleftsv The implants are splinted together with an implant supported connecting barv An removable partial denture supported anteriorly by implants and posteriorly by the remaining molars
- 123. Zygomaticus implants for cleftsl An overlay RPD was fabricated for the maxilla and an overlay complete denture for the mandiblel Note the lip support provided by the prosthesis
- 124. Zygomaticus implants for cleftsa b cd e f ga: Edentulous patient with repaired bilateral cleft.b,c: Four implants have been placed, two conventional and two zygomaticus types.d: Implant supported implant connecting.e: Prosthesis.f: Prosthesis in place. Note obturator extension. g: Final result.
- 125. Overlay Removable Partial DenturesUsual clinical findings v Collapsed maxillary arches v Inadequate alveolar development v Excessive inter-occlusal space v Retarded growth of the maxilla
- 126. Overlay Removable Partial Dentures Purpose of the prosthesis ” Restore the missing dentition ” Restore the vertical dimension of occlusion ” Provide support and contour for the upper lip
- 127. Overlay Removable Partial DenturesPurpose” Restore the missing dentition” Restore the vertical dimension of occlusion” Provide support and contour for the upper lip. Note the thickness and contour of the labial flange
- 128. Overlay Removable Partial DenturesImportant note: ” Before making preliminary or master impressions carefully inspect the repaired cleft for fistulas. These areas must be carefully blocked out with gauze prior to making impressions in order to prevent impacting impression materials within the nasal cavity.
- 129. Overlay Removable Partial Dentures” If the interocclusal distance is excessive and the VDOoverclosed, an improved vertical dimension of occlusion canbe established with selective crown placement
- 130. Overlay Removable Partial DenturesCopings on premolars to These copings will be enclosedbe overlayed protect within the overdenture.these teeth from caries. Crown contours are made ideal for the partial overdenture framework.
- 131. Overlay Removable Partial DenturesNote the thickness ofthe labial flange. The processed overdenture with the border molded soft palate obturator. These copings are incorporated within the overlay denture.
- 132. Overlay Removable Partial Dentures Note: l Anterior open bite l Fistulas l Soft palate defect
- 133. Overlay Removable Partial Denturesv Remaining teeth covered with gold copings.v Tooth tissue junction should be covered with metal as opposed to acrylic resinv Implants placed in posterior quadrant.
- 134. Overlay Removable Partial Dentures Border molding the soft palate portionThe obturator portion is developed with compound and thermoplasticwax. (see “Restoration of soft palate defects” FFOFR.org for details).
- 135. Design of the metal framework” Note that the tooth tissue junction of all overlaid teeth are covered with metal as opposed to acrylic resin. The resin is porous and if you cover these areas with this material you will increase the risk of gingival caries” Note the metal occlusal surfaces overlaying the implant connecting bar. This was done to accommodate for the lack of space between the implant connecting bar and the opposing natural dentition.
- 136. Overlay Removable Partial Dentures Definitive prosthesis.
- 137. Overlay Removable Partial DenturesThe premaxilla of this patienthas been removed. Note thefistula anteriorly. This mustbe carefully occluded withgauze before makingimpressions. The maxillarymolars were restored with fullveneer crowns to restore theVDO to a proper level.The premolars were covered with copings and splinted tothe first molars. The prosthesis will overlay these copings.Note the ERA attachments (arrows). These attachmentsretain the prosthesis but disengage when incisal forcesare delivered. The axis of rotation is determined by thedistal rests on the first molars bilaterally (arrows).
- 138. Overlay Removable Partial Dentures This cleft was not bone grafted and therefore the individual segments move independent of one another exposed to the forces of mastication. Therefore cleft segments have not been united prosthodontically.
- 139. Overlay Removable Partial DenturesThe prosthesis inserted. Circumferential claspshave been used. Note the anterior overlay.
- 140. Overlay Removable Partial DenturesThe anterior overlay restores the anterior dentition,provides lip support and obturates the anteriorfistula.
- 141. Role of Osseointegrated ImplantsImplants can provide cleft patients significant benefit particularly thoserestored with an overlay prosthesis. This patient has retained only themaxillary 2nd molars. The removable partial denture she was wearingrestored the missing dentition and provided support for the lip but lackedanterior support. Implants provided the needed support.
- 142. Role of Osseointegrated ImplantsA lateral cephalogram indicated sufficient bone availableanteriorly and implants were place on both sides of thecleft. Note that the premaxilla had been removedpreviously.
- 143. Role of Osseointegrated ImplantsA “Hader bar” and an “O” ring type attachment wereuse to retain the overlay prosthesis. The occlusal surfaces of the mandibular teeth were altered to alleviate occlusal plane discrepancies.
- 144. Role of Osseointegrated ImplantsThe finished prosthesis in position. The posterior mandibulardentition was restored with a removable partial denture. Thecleft segments had not been grafted together an so theywere not splinted with the implant apparatus.
- 145. Obturating residual soft palate defects not previously obturated” Speech will remain hypernasal but leakage during swallowing will be reduced.” Long standing errors in articulation remain.
- 146. v Visitffofr.org for hundreds of additional lectures on Complete Dentures, Implant Dentistry, Removable Partial Dentures, Esthetic Dentistry and Maxillofacial Prosthetics.v The lectures are free.v Our objective is to create the best and most comprehensive online programs of instruction in Prosthodontics


 Restoration of Posterior Quadrants and Treatment Planning
Restoration of Posterior Quadrants and Treatment Planning
 Angled Implants
Angled Implants
 Prosthodontic Procedures and Complications
Prosthodontic Procedures and Complications
 Computer Guided Treatment Planning and Surgery
Computer Guided Treatment Planning and Surgery
