The goals of the obturator prosthesis are to restore the partition between the nasal and oral cavities, restore palatal contours, restore midfacial contours compromised by the surgical resection, restore speech and swallowing and replace the missing dentition. These goals can almost always be met when good communication exists between the oncologic surgeon and the prosthodontist. The result will be the creation of surgical defects that are better suited for the prosthesis without compromising the resection of the tumor. This program discusses these surgical enhancements (for example – skin grafting the raw tissues in the defect) in considerable detail and illustrates the gains that can be achieved when they are employed.
Maxillofacial Prosthetics – Palatal Resections – Alterations at Surgery to Enhance the Prosthetic Prognosis — Course Transcript
- 1. 11. Palatal Resections – Alterations at Surgery to Enhance the Prosthetic Prognosis John Beumer III, DDS,MS Distinguished professor emeritus UCLA School of Dentistry
- 2. Maxillary Defects – Prosthodontic ChallengesDentulous patients Restore the partition between the oral and nasal cavitiesRestore palatal contours Replace needed dentition Provide retention, stability, support for the partial denture-obturator prosthesis Create partial denture designs that do not stress abutment teeth beyond their physiologic tolerance
- 3. Maxillary Defects – Prosthodontic ChallengesEdentulous patients Restore partition between the nasal and oral cavities Restore palatal contours Replace the necessary dentition Provide retention, stability, and support for the complete denture – obturator prosthesisTo meet these challenges we need the help andcooperation of our surgical oncology colleagues.
- 4. Maxillary Defects – Prosthodontic Challenges Edentulous patients Restore partition between the nasal and oral cavities Restore palatal contours Replace the necessary dentition Provide retention, stability, and support for the complete denture – obturator prosthesisThe surgeon can help by creating an accessible, skinlined defect that can be used to help retain, stabilized,and support the future obturator prosthesis.
- 5. Alterations at Surgery to Enhance the Prosthetic Prognosis Skin grafting the defect Maintain access to the defect Salvaging the premaxillary segment Soft palate resection and velopharyngeal function Retention of key teeth Use of palatal mucosa Placement of osseointegrated implants
- 6. Skin Grafting – Advantages In radical maxillectomy defects skin grafting the inside of the cheek flap creates a divergent lateral wall which when engaged by the obturator prosthesis, facilitates retention. The scar band at the skin graft mucosal junction creates an undercut superior to this junction . Engagement of this undercut with the obturator prosthesis facilitates retention on the defect side. A skin lined cheek flap is more flexible than one that epithelializes spontaneously and can be more effectively displaced by the prosthesis allowing for the development of better midfacial contours on the defect side. Skin lined defects provide keratinized surfaces in the defect that can be engaged more aggressively with the prosthesis thereby improving stability, retention and support for the obturator prosthesis.
- 7. Skin graftingNote the undercut just superior to the skin graft mucosaljunction (arrows). In addition, the lateral walls of theseskin lined defects diverge superiorly and if properlyengaged, retention of the obturator prosthesis issignificantly enhanced.
- 8. Skin grafting vs spontaneous epithelialization Note the difference between these two defects. The defect on the left is lined with skin and can be aggressively engaged prosthodontically enhancing stability, retention and support. The defect on the right is lined with poorly keratinized squamous epithelium and respiratory epithelium. Neither of these epithelial surfaces are suited to resist the abrasion associated with the use of an obturator prosthesis.
- 9. Skin grafting vs spontaneous epithelialization Both these patients had similar resections. In one a skin graft was used to line the defect. In the other, the wound was allowed to epithelialize spontaneously. The skin lined defect can be used to help support, stabilize, and retain the obturator prosthesis whereas the defect without skin lining cannot be so utilized .
- 10. Skin grafting vs spontaneous epithelialization Total palatectomy defectsAlthough large, such defects can be restored prosthodontically ifskin lined. In this patient there were soft tissue undercutsbilaterally and these were engaged by using a two pieceprosthesis providing the patient with a well retained obturatorprosthesis. Speech and swallowing were fully restored butmastication was still severely compromised.
- 11. Total palatectomy defects Two piece obturator prosthesis This type of prosthesis is effective in restoring speech and swallowing but mastication will be severely compromised.
- 12. Skin grafting vs spontaneous epithelialization Total palatectomy defectsThis defect was not lined with skin and has undergonecontraction. Unfortunately, it is not restorable usingprosthodontic means.
- 13. Skin grafts vs secondary epithelializationEven though these patients are edentulous their defects arerelatively easy to obturate because the defects are lined withskin. Properly engaging the lateral wall of the defect and theundercut just superior to the skin graft mucosal junction willgreatly facilitate the retention and stability of the obturatorprosthesis.
- 14. Skin grafting vs spontaneous epithelialization Grafting this defect prevented undesirable contraction of the upper lip and it retains much of its original flexibility. The result: A properly extended obturator prosthesis will restore the contours of the upper lip.
- 15. Anterior defects Skin lined defects vs defects which are allowed to granulate and epithelialize spontaneouslyAdvantages of skin lined anterior defectsb) Improved support provided by the defectc) Less contraction of the lipd) More control over the lip contours with the obturator prosthesis
- 16. Skin graft vs Secondary Epithelialization This wound was closed primarily and the raw tissue surfaces were not skin grafted.Result: The upper lip contracted and normal lip contours couldnot be restored with the labial flange of the prosthesis.
- 17. Anterior defectsa b An attempt was made to close this defect primarily. Note scarring and lip retraction that results.
- 18. Skin grafts vs spontaneous epithelializationNote the poor quality tissues in the defect. Defects such asthese are difficult to restore because the defect can not beproperly engaged with the obturator extension.Result: The retention and stability of the prosthesis iscompromised.
- 19. Skin grafts vs secondary epithelializationThe skin graft placed into this defect sloughed and the wound epithelializedwith poorly keratinized epithelium and respiratory epithelium. This type ofmucosal lining does not tolerate well the abrasion associated with the wearof an obturator prosthesis. In addition, because of contraction of the defectand the lack of a skin graft mucosal junction there are no undercuts toengage.Result: Retention and stability are compromised.
- 20. Access to the defect Large defects should not be closed surgically and access to the defect should be maintained.An attempt was made to close this defect primarily. This defectcan be obturated but the forces of gravity and the long lever armof the prosthesis will place great stress and strain on the abutmentteeth which could lead to their premature loss.
- 21. Access to the defect must be maintained In this patient the middle turbinates were retained. They subsequently became edematous and extended down into the oral cavity, distorted the palatal contours of the obturator prosthesis, violating the tongue space. They were subsequently removed.
- 22. Access to the defect must be maintained This defect was closed with a flap. Note the distortion of the palatal contours and the elimination of the tongue space. This patient could not be fitted with a prosthesis. He was unable to masticate and his speech articulation was severely compromised.
- 23. Access to the defectThis defect was closed with a radial forearm free flap. Note thedistortion of the palatal contours and the compromise of thetongue space. Absent the retentive contribution of the defect, thepartial denture restoring the posterior dentition delivers clinicallysignificant stress to the abutment teeth.
- 24. Access to the defectResult:Over time the teeth retaining this partial denture and obturatormay be lost prematurely.In addition, the patient complained about the accumulation ofsecretions in the nasal cavity on the defect side.
- 25. Access to the defectProblems as a result of these mucous accumulations:b) Local infections.c) A very strong and unpleasant odor emanating from the nasal passages on the defect side.
- 26. A Retention of the premaxilla: Advantages-Edentulous Patients Improved support because of increased palatal shelf surface area B Improved stability Additional implant sitesIn patient “B” only a small portion of the premaxilla on the defect side wasretained, but as a result significant amounts of palatal shelf were savedleading to increased support for the obturator prosthesis.
- 27. Retention of the premaxilla: Advantages-Edentulous Patients In this patient sufficient bone remained to permit the placement of three implants.
- 28. Retention of the premaxillaAdvantages in partially edentulous patients Retaining the premaxilla on the defect side allows for more favorable partial denture designs Rests can be positioned so that occlusal forces can be directed along the long axis of the abutment teeth.
- 29. Retention of the premaxillary segmentWhen the premaxillary segment has been completelyremoved, support is significantly compromised and thepartial denture framework will expose the remaining teethto clinically significant lateral forces.
- 30. Retention of the premaxilla Implant sitesThe best implant site in the upper jaw is the premaxilla. In mostmaxillectomy patients, 2-4 implants can be placed in this region.The more of the premaxilla available for implant placement themore favorable the implant distribution pattern (A-P spread).
- 31. Retention of key abutment teethAbutment teeth adjacent to the defect are subjected to thegreatest stress and bony cuts through the alveolus next to theseteeth should be interproximal rather than intraseptalIn this patient the transalveolar bony cut was properly made.The result: This abutment tooth is circumscribed by alveolarbone, making it a suitable partial denture abutment.
- 32. Retention of key abutment teethIn these three patients bony cuts through the alveoluswere made too close to the roots of teeth. The result:These teeth are of limited value as partial dentureabutments for the obturator prosthesis.
- 33. Soft palate resection and velopharyngeal closure Middle third of the soft palate is responsible for palatal elevation (levator veli palatini) during velopharyngeal closure. In partially edentulous patients when teeth can effectively retain the obturator prosthesis, when the middle third is resected for tumor control the remaining posterior third should also be resected. This will insure appropriate access to the residual velopharyngeal musculature. In edentulous patients, when difficulty with retention is anticipated, these nonfunctional posterior one third remnants are retained to facilitate retention.
- 34. Soft palate resection and velopharyngeal closure Remnants of the levator are generally present and functional after complete removal of the soft palate. These muscle remnants are imbedded within the lateral wall of the pharynx and their contracture plus contraction of the superior constrictor comprise the residual velopharyngeal mechanism. the obturator to restore In order for speech to normal the obturator extension must interact with this residual musculature in a precise manner. Retaining nonfunctional soft palate remnants may make it difficult to achieve this precise interaction.
- 35. Soft palate resectionThe posterior one third of the soft palate was retained in boththese patients. This strip of mucosa is nonfunctional andprevents proper extension an precise placement of an obturatorprosthesis into the residual, still functional velopharyngealmechanism. Result: Speech will be hypernasal.
- 36. Soft palate resection and velopharyngeal closure In edentulous patients the needs of retention outweigh the needs of precise velopharyngeal closure Extension onto the nasal side of the residual soft palateIn this patient the soft palate remnant was retained because itcan be used to aid retention of the obturator prosthesis.
- 37. Palatal mucosa The palatal margin of the defect is a fulcrum around which the prosthesis rotates, particularly in edentulous patients. When possible this bony margin should be covered with palatal mucosa as was done in these two patients. Bony cut Palatal incision
- 38. Placement of osseointegrated implantsimmediately following resection of the tumorConsidered: In edentulous patients When the prognosis for the remaining dentition is poor
- 39. Placement of osseointegrated implantsimmediately following resection of the tumorin patients to receive postoperative radiation Inpatients scheduled to receive postoperative radiation therapy the dose enhancement effect at the bone implant interface is outweighed by the bone anchorage achieved during the 6 week postoperative period prior to commencement of radiation therapy.
- 40. Rehabilitation – Surgery vs ProsthodonticsArguments in favor of prosthodontic rehabilitation It is more cost effective The open defect can be monitored for tumor recurrence Bulky flaps distort palatal contours and reduce the tongue space compromising speech articulation and control of the bolus during mastication. Palatal contours and speech articulation are best restored with an obturator prosthesis Mucous tends to accumulate on the nasal side of the flap causing unpleasant odors and local infections Partial denture designs and stresses on abutment teeth Inability to use the defect to facilitate retention on the side of the defect results in additional stresses on the residual dentition leading to premature loss of abutment teeth.
- 41. Surgery vs Prosthodontics (cont’d) Small defects in dentulous patients Small defects, secondary to removal of benign tumors, such as this one, can be closed without distorting palatal contours. This patient played a reed instrument and although her speech was normal, she could not play effectively with an obturator prosthesis. The tumor was benign, a suitable followup period had elapsed, and so the defect was closed with local flaps.Note: A partial denture was still needed to restorethe missing molar dentition.
- 42. Surgery vs Prosthodontics Large defects are best restored prosthodontically This defect was closed with a radial forearm flap. A prosthesis was still necessary for esthetics, lip support, and to prevent supereruption of the opposing mandibular dentition . Without, the benefit of the retentive qualities of the defect however, the abutment teeth, particularly the cuspid may be exposed to forces beyond the physiologic limits of the periodontal ligament.Following reconstruction the patient complained of a foul odor coming from thesinus. Exam revealed significant accumulations of dried mucous on the sinusside of the flap which could not be easily removed by the patient.
- 43. Surgery vs Prosthodontics This large maxillectomy – orbital exenteration defect was restored with radial forearm flap combined with an orbital prosthesis and a maxillary obturator prosthesis. Note that the maxillary defect was not obliterated by the flap. The obturator prosthesis replaces the missing teeth, and restores palatal contours. Speech articulation is normal and hypernasality is eliminated.
- 44. Surgery vs Prosthodontics Selected maxillary defects can be effectively reconstructed with vascularized free flaps. This technique is generally best suited for secondary reconstruction after the patient is proven to be free of disease. The defect must be of sufficient size because the vascularization of small free flaps with bone grafts of less than 2 cm is not predictable
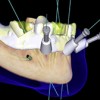
- 45. Surgery vs Prosthodonticsa b cd e gh a. Surgical defect. b and c. Drill guide secured, implant sites prepared and osteotomies completed. d and e. Graft secured in position. f and g. Occlusion of fixed partial denture. Note palatal contours are near normal. Courtesy Dr. D. Rohner and Dr. H. Reintsema
- 46. Visit ffofr.org for hundreds of additional lectures on Complete Dentures, Implant Dentistry, Removable Partial Dentures, Esthetic Dentistry and Maxillofacial Prosthetics. The lectures are free. Our objective is to create the best and most comprehensive online programs of instruction in Prosthodontics


 Prosthodontic Procedures and Complications
Prosthodontic Procedures and Complications
 Single Tooth Defects in Posterior Quadrants
Single Tooth Defects in Posterior Quadrants
 Computer Guided Treatment Planning and Surgery
Computer Guided Treatment Planning and Surgery
 Cement Retention vs Screw Retention
Cement Retention vs Screw Retention
