Implant Dentistry – Stage I and II Surgery – Presentation Transcript
- 1. Dental Implant Surgery Stage I & II Procedures Moustafa El-Ghareeb BDS, MS Associate Clinical Professor Oral & Maxillofacial Surgery This program of instruction is protected by copyright ©. No portion of this program of instruction may be reproduced, recorded or transferred by any means electronic, digital, photographic, mechanical etc., or by any information storage or retrieval system, without prior permission.
- 2. Osseointegration A direct structural and functional connection between ordered, living bone and the surface of a load-carrying implant (Brånemark, 1985) Cortical bone Cancellous bone Per-Ingvar Brånemark
- 3. Osseointegration Micromotion at the bone-implant interface beyond 150 μm results in fibrous encapsulation instead of osseointegration (Szmukler-Moncler et al. 1998)
- 4. Osseointegration Osseous Healing: • • • • • • • • Blood fills gap between implant and damaged bone surface Blood clots with fibrin network formation (Platelets) Inflammation (PMN s & Macrophages) Resorption (Macrophages ingest inflammatory debris & Osteoclasts resorb damaged bone ) Neovascularization (Endothelial cells) Migration/differentiation/ proliferation (MSC s, fibroblasts & osteoblasts) Osteoid & Woven bone (osteoblasts) 4-6 weeks after surgery Replacement of woven bone by lamellar bone (osteoclasts & osteoblasts) Basic multi-cellular unit Osteoclast cutting cone: basic remodeling process for bone renewal
- 5. Osseointegration Osseous Healing: Distant Osteogenesis only Machined Smooth Surface Contact & Distant Osteogenesis Rough or Enhanced Surface Improves Cell Attachment
- 6. Osseointegration Enhanced Surfaces: • Acid etched • Sand blasted Subtractive • Titanium oxide blasted Additive • HA coated • Anodized SLA® Acid Etched TiUnite® TiOblast™
- 7. Peri-Implant Soft Tissue Healing & Biology • Bone resorption occurs to create a proper soft tissue seal around implants • The term biologic width is used when describing the soft tissue dimensions around implants • Epithelial cells are attached by hemidesmosomes & basal lamina • Collagen fibers are oriented parallel to the implant surface CTA
- 8. Osseointegration Original Brånemark Protocol • • Implants must be sterile Made of highly biocompatible material such as titanium (covered by a biologically inert TiO2 layer) • Inserted with atraumatic surgical technique that avoids overheating of bone • Implants must have good initial stability at the time of placement • Implants must not be subjected to functional forces during initial healing period A non-loaded healing period: 1. Anterior MN: 3 m 2. Posterior MN: 4 m 3. Maxilla: 6 m Submerged & Non-loaded
- 9. Traditional Loading Maxilla: 6 months Ant MN: 3 months Post MN: 4 months Two-Stage Cover Screw Stage 1 Surgery Healing Abutment Stage 2 Surgery One-Stage Final Restoration Healing Abutment Final Restoration
- 10. Surgical Considerations • • • • • Informed consent signed Preoperative ABx Chlorhexidine mouth rinse Standard sterile technique Atraumatic surgical technique: 1. Sharp clean incisions 2. Appropriate flap design 3. Sharp drills 4. Copious irrigation 5. Intermittent moderate speed (<2,000 rpm) 6. Gentle handling of tissue Sharp Clean Incision H incision Flap Design ‘Papilla-sparing Incision’
- 11. Surgical Considerations • • • • • Excessive surgical trauma and thermal injury result in osseonecrosis and fibrous encapsulation Temperature over 47 °C for 1 min causes heat necrosis in bone (Eriksson & Albrektsson 1983) Heat generation is affected by speed, load placed on drill, drill sharpness and design Precise osteotomy preparation by surgeon to achieve good primary stability Good primary closure 47 °C Precise osteotomy preparation Good Primary Closure From Larry Peterson, Contemporary Oral & Maxillofacial Surgery, 3rd Edition
- 12. Surgical Considerations Implant Design • • Primary mechanical stability is provided by implant design, bone quality & precise osteotomy preparation The transition from primary mechanical stability to biologic stability takes place during early wound healing & is provided by newly formed bone Threaded Implant Cylinder-Type Implant Press-fit Precise Osteotomy Preparation
- 13. Stage One Surgery • When to tap? • When to countersink? • Coolant (copious irrigation) • Sharp drills • Temp over 47 °C for 1 min causes heat necrosis in bone (Eriksson & Albrektsson 1983) • Up & down motion for effective irrigation • Avoid over-torque (Implant over-tightening causes bone micro-fractures/bone necrosis)
- 14. Stage One Surgery • Twist drills are longer than selected implants • Countersink only in presence of thick cortical layer • Excessive countersinking in poor quality bone may compromise primary stability • Tap only in dense bone (most implants are self tapping i.e. self threading) • Placement torque should not exceed 45 Ncm
- 15. Anatomical Considerations 5.0 mm Mental Nerve IAN 2 mm 3 mm Mental Nerve exiting without Anterior Looping Mental Nerve Anterior Looping
- 16. Anatomical Considerations Heasman 1988 Rajchel et al 1986 IAN IAN Lingual Nerve Lingual Nerve Wilson 1989
- 17. Anatomical Considerations Nasal Cavity & Maxillary Sinus
- 18. Anatomical Considerations Alveolar Bone Contours Labial Concavity Lingual Concavity Lingual plate perforation Lingual Artery: Hemorrhage Lingual Nerve: Nerve damage
- 19. How to Assess Implant Primary Stability? 1. • • • • Resonance Frequency Analysis (RFA)/Implant Stability Quotient (ISQ) Transducer is excited over a frequency range Response is measured RF is determined by degree of stiffness at IBI & level of bone surrounding the implant Implant stability quotient (ISQ) is a numerical value ranging from 0 – 100 reflecting the level of stability
- 20. How to Assess Implant Primary Stability? 2. Implant insertion torque
- 21. Stage Two Surgery • Implant exposure • Removal of cover screw • Selection of healing abutment: A periodontal probe determines ST thickness • Connection of healing abutment using a screw driver Abutments have to be fully seated Cover screw exposure Abutments emerge from ST by about 1-2 mm
- 22. One-Stage Versus Two-Stage Things to consider: • Primary stability • Interim prosthesis (can it be modified without weakening) • Patient compliance • Placement of implants & simultaneous grafting e.g. guided bone regeneration (GBR) Implant placed as a two-stage Implant placed as a one-stage
- 23. One-Stage Versus Two-Stage When to consider one-stage placement? 1. The implant has good primary stability 2. The interim prosthesis can be modified to accommodate the healing abutment 3. Implant placement is associated with no grafting or minimal grafting
- 24. Extraction & Immediate Implant Placement Evaluation at the time of C/S 1. Smile line (SL) Ø 2. Gingival Biotype (GB) Ø 3. 4. 5. Avoid in thin scalloped GB as it is usually associated with thin labial bone plate Infection-free site Inflammation-free site Check radiographically for proximity of apex of socket to vital structures e.g. IAN, Maxillary sinus &Nasal cavity Ø 6. Avoid in high SL Avoid if there is proximity Look for features that lead to good primary stability e.g. short and small roots, wide inter-radicular bone, small tooth size (molars vs. bicuspids vs. incisors) Thin Scalloped Thick Blunted
- 25. Extraction & Immediate Implant Placement Evaluation at the time of extraction 1. Atraumatic extraction 2. Check height & thickness of labial or buccal plate of bone 3. Check morphology of socket and gap between implant & socket wall (<2mm no grafting, >2mm graft) 4. Primary stability Ø Avoid if you cannot get good primary stability
- 26. Thank you
- 27. v Visit ffofr.org for hundreds of additional lectures on Complete Dentures, Implant Dentistry, Removable Partial Dentures, Esthetic Dentistry and Maxillofacial Prosthetics. v The lectures are free. v Our objective is to create the best and most comprehensive online programs of instruction in Prosthodontics


 Single Tooth Defects in Posterior Quadrants
Single Tooth Defects in Posterior Quadrants
 Restoration of Posterior Quadrants and Treatment Planning
Restoration of Posterior Quadrants and Treatment Planning
 Angled Implants
Angled Implants
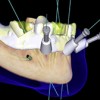 Computer Guided Treatment Planning and Surgery
Computer Guided Treatment Planning and Surgery
